Current Issue Volume 10, Issue 2 - 2025
The Role of ECG in Differentiating Arrhythmogenic Cardiomyopathy and Uhl Anomaly
Stefan Peters*
Medical Care Unit Elze, Cardiology, Germany
*Corresponding Author: Prof.Dr.med. Stefan Peters, Medical Care Unit Elze, Cardiology, Königsberger Str. 1, 31008 Elze, Germany, Tel: +49 5068 9337022, Email: [email protected]
Received Date: March 11, 2025
Published Date: April 04, 2025
Citation: Peters S, et al. (2025). The Role of ECG in Differentiating Arrhythmogenic Cardiomyopathy and Uhl Anomaly. Mathews J Case Rep. 10(2):203.
Copyrights: Peters S, et al. © (2025).
ABSTRACT
The role of standard ECG in differentiating Uhl anomaly and arrhythmogenic cardiomyopathy is not easy to define. According to Padua criteria low voltage in limb leads and T-wave inversions in inferolateral or lateral leads as minor criteria arrhythmogenic cardiomyopathy can be defined as biventricular, right dominant or left dominant form of the disease. Here, this is discussed in details.
Keywords: Low Voltage in Limb Leads, T-Wave Inversion in Inferolateral of Lateral Leads, Uhl Anomaly, Arrhythmogenic Cardiomyopathy, Cardiac Sarcoidosis.
INTRODUCTION
Uhl anomaly is a rare disease with a prevalence of 1:1000000 inhabitants. There are about 50 – 60 patients described in the literature. ECG findings vary a lot from right bundle branch block, QRS fragmentation to unspecific changes of repolarisation.
Low voltage in limb leads as a minor depolarisation criterium and T-wave inversions in inferolateral or lateral leads as a minor repolarisation criterium helps to define different aspects of certain diseases.
As a starting point serves a 18-year-old male patient with the echocardiographic and cardiac MRI diagnosis of Uhl anomaly and no complaints.
METHOD
The ECG of this single patient was compared to typical ECG findings in arrhythmogenic cardiomyopathy, either with right ventricular dominance, biventricular or left ventricular dominance, and cardiac sarcoidosis.
RESULTS
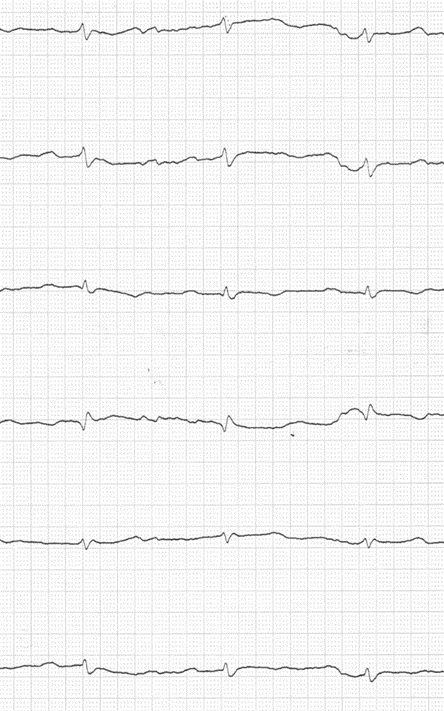
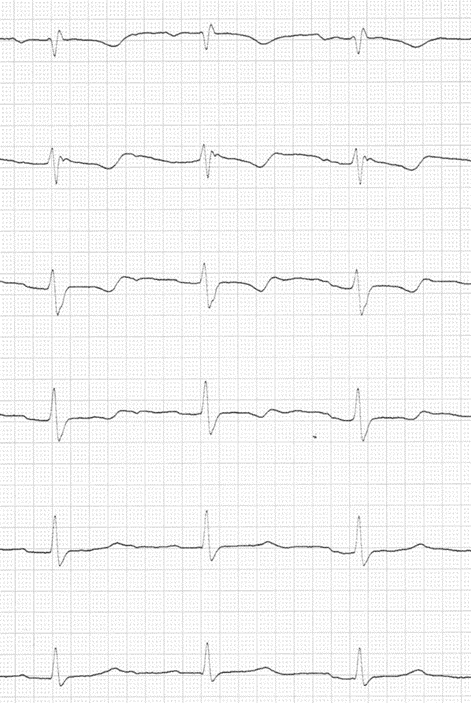
The ECG of the single patient with proven Uhl anomaly revealed sinus rhythm, low voltage in limb leads, and T-wave inversions in inferior and chest leads in lead V1 to V5/V6. The ECG in Uhl anomaly is shown in figure 1. The configuration of the ECG resembles typical ECG changes in arrhythmogenic left ventricular cardiomyopathy except that T-wave inversions are anterolateral in lead V1 to V5 (V6). The only mutation that leads to much higher turn-off (lead V3 to V6, in some cases V2 to V6) is phospholamban. A typical example of phospholamban mutation is presented in figure 2. In phospholamban mutations the progression to complete right bundle branch block with T-wave inversions in right or left precordial leads is a well-known phenomenon. T-wave inversions in right and left precordial leads as a sign of arrhythmogenic biventricular cardiomyopathy, often treated with heart transplantation. The ECG of a case treated with heart transplantation is shown in figure 3. In the case of Uhl anomaly the function of the left ventricle was completely normal due to echocardiography with no late enhancement in cardiac MRI.
Figure 1. ECG of the 18-year-old patient with Uhl anomaly with low voltage in limb leads, epsilon waves and QRS fragmentation in lead V1, and T-wave inversion in lead II, III, aVF and in lead V1 to V5. Localized right precordial QRS prolongation and terminal activation delay are missing.
Figure 2. Typical ECG of arrhythmogenic left ventricular cardiomyopathy in phospholamban mutation with low voltage in limb leads, T-wave inversions inferior and in chest leads V3 (V2) to lead V6.
Figure 3. Typical ECG of developing right bundle branch block, low voltage in limb leads, and T-wave inversions in lead V1 to V5 as a hint of arrhythmogenic biventricular cardiomyopathy treated with heart transplantation.
DISCUSSION
In Uhl anomaly due to small numbers of case reports a unique ECG pattern does not exist. In the single 18-year-old patient the ECG resembles arrhythmogenic left ventricular cardiomyopathy with inferior T-wave inversions, low voltage in limb leads, and T-wave inversions anterolateral. The T-wave inversions anterolateral are precisely the difference to arrhythmogenic left ventricular cardiomyopathy. Similarities exist to phospholamban mutations as the cause of arrhythmogenic left ventricular cardiomyopathy [1], differencies exist with no late enhancement of the left ventricle. Arrhythmogenic left ventricular cardiomyopathy can be clearly ruled out.
The next option is arrhythmogmenic biventricular cardiomyopathy. The ECG of the patient resembles this option, too. In the course of arrhythmogenic right ventricular cardiomyopathy progressive left ventricular disease leads not only to progressive T-wave inversions in chest leads, but also to T-wave inversions in inferior leads. The most differential diagnosis seems to be arrhyhmogenic biventricular cardiomyopathy, but an echocardiographic and MRI prove that the left ventricle is affected is missing.
Another differential diagnosis is arrhythmogenic right ventricular cardiomyopathy with typical ECG findings like localized right precordial QRS prolongation [2], epsilon waves [3], terminal activation delay [4], the phenomenon of the amplitude of T-wave inversion in lead V1 > V2 (due to experiences with bipolar chest leads in arrhythmogenic right ventricular cardiomyopathy [5]), T-wave inversions only in right precordial leads [6], right precordial QRS fragmentation [7], and typical findings in lead aVR [8]. Due to electroanatomic scar the Q wave in lead aVR is large, due to myocardial atrophy the R wave in lead aVR is small, and the amplitude of inverted T-waves ≤ 2mm due to both phenomenons. The sensitivity of localized right precordial QRS prolongation is 98%, and the sensitivity of the described changes in lead aVR even 100% in large collective of 490 patients [9].
The last option is right ventricular sarcoidosis. Typical ECG findings are: right precordial T-wave inversions, low voltage in limb leads, epsilon waves, atrioventricular conduction abnormalities, and precordial R‘ waves [10]. The ECG of the patient reveals three positive criteria, only atrioventricular conduction abnormalities and significant precordial R‘ wave are missing. A typical example of cardiac sarcoidosis is presented in figure 4. In cardiac MRI, however, there is no hint of right ventricular sarcoidosis.
Figure 4. Typical ECG in cardiac sarcoidosis with low voltage in limb leads, right precordial T-wave inversion and epsilon waves, atrioventricular block and significant precordial R‘ wave.
CONCLUSION
ECG findings help to differentiate between certain forms of right ventricular abnormalities like arrhythmogenic cardiomyopathy with right dominant, biventicular and left dominant appearance and Uhl amomaly.
Nevertheless, the ECG of the patient suggests that Uhl anomaly seems to be a maximum variant of arrhythmogenic right ventricular cardiomyopathy, although differences (no fatty infiltration, no right ventricular aneurysms or trabecular structure) exist. This suggestion cannot be proven or excluded due to a rather small number of patients with described ECG findings.
REFERENCES
- Peters S. (2021). History of phospholamban mutation in arrhythmogenic cardiomyopathy: a case report. Mod Appl Med Res. 1(5):04-05.
- Peters S, Trümmel M. (2003). Diagnosis of arrhythmogenic right ventricular dysplasia-cardiomyopathy: value of standard ECG revisited. Ann Noninvasive Electrocardiol. 8(3):238-245.
- Wang J, Yang B, Chen H, Ju W, Chen K, Zhang F, et al. (2010). Epsilon waves detected by various electrocardiographic recording methods: in patients with arrhythmogenic right ventricular cardiomyopathy. Tex Heart Inst J. 37(4):405-411.
- Cox MG, van der Smagt JJ, Wilde AA, Wiesfeld AC, Atsma DE, Nelen MR, et al. (2009). New ECG criteria in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Arrhythm Electrophysiol. 2(5):524-530.
- Batchvarov VN, Bastiaenen R, Postema PG, Clark EN, Macfarlane PW, Wilde AA, et al. (2016). Novel electrocardiographic criteria for the diagnosis of arrhythmogenic right ventricular cardiomyopathy. Europace. 18(9):1420-1426.
- Marcus FI, Fontaine G. (1995). Arrhythmogenic right ventricular dysplasia/cardiomyopathy: a review. Pacing Clin Electrophysiol. 18(6):1298-314.
- Peters S, Truemmel M, Koehler B. (2012). Prognostic value of QRS fragmentation in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. J Cardiovasc Med (Hagerstown). 13(5):295-298.
- Peters S. (2014). Clinical importance of lead aVR in arrhythmogenic cardiomyopathy. Int J Cardiol. 176(2):508-509.
- Peters S. (2023). Electroanatomic scar and myocardial atrophy in arrhythmogenic cardiomyopathy: review of ECG criteria. Ann Cardiol Vasc Med. 6:1075.
- Hoogendoorn JC, Venlet J, Out YNJ, Man S, Kumar S, Sramko M, et al. (2021). The precordial R' wave: A novel discriminator between cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy in patients presenting with ventricular tachycardia. Heart Rhythm. 18(9):1539-1547.
.png)
.png)
.png)