Previous Issues Volume 9, Issue 1 - 2024
The Impact of Family-Centered Care Training: Developed Pediatric Nurses' Attitudes towards Child Care in Turkey
Ayfer Kara1,*, Fatma Guducu Tufekci2
1Assistant Professor, Sutçu Imam University, Health Science Faculty, Kahramanmaraş, Turkey
2Associate Professor, Ataturk University, Faculty of Nursing, Erzurum, Turkey
*Corresponding author: Ayfer Kara, PhD, Department of Child Health and Diseases Nursing, Health Science Faculty, Sütçü Imam University, 46040, Kahramanmaraş, Turkey, Phone Number: 05069894558, ORCID: 0000-0003-3408-9771; Email: [email protected].
Received Date: January 10, 2024
Published Date: February 06, 2024
Citation: Kara A, et al. (2024). The Impact of Family-Centered Care Training: Developed Pediatric Nurses' Attitudes towards Child Care in Turkey. Mathews J Pediatr. 9(1):33.
Copyrights: Kara A, et al. © (2024).
ABSTRACT
Aim: This study was conducted to improve the attitudes of pediatric nurses towards family-centered care through education and to evaluate the effectiveness of this education. Methods: The study was conducted quasi-experimental with pretest-posttest control group in order to evaluate the effect of family-centred care training on the care attitudes of paediatric nurses. The study was conducted between January 15 and April 15, 2018. The population of the study consisted of 63 nurses (N= 63). The data were collected face-to-face through the Descriptive Characteristics Form and the Family Centered Care Attitude Scale. The data were analysed through descriptive statistics, chi-square, t test and z test. Ethical principles were observed at all stages of the study. Results: The results of the research indicated that attitudes of the nurses in the experimental group towards family-centred care, contribution of family-centred care subscale and family and child participation in care subscale were significantly higher in the experimental group compared to the nurses in the control group after family-centred care training (p <.001). Conclusions: Pediatric nurses play a key role in en-abling hospital care services to become family-centered. Training of nurses, working in paediatric clinics, on family-centred care may be effective in improving their attitudes towards family-centred care.
Keywords: Family-Centred Care, Child, Training, Nurse, Attitude.
INTRODUCTION
Pediatric nurses play an important role in the healthy growth and development of children, including physical, cognitive, emotional, and social. Nurses protect children from diseases, maximize their health, and provide treatment, care, and rehabilitation. Nurses often collaborate with family members to fulfill their responsibilities and meet the child’s needs, thus improving healthcare outcomes. Family participation in child care not only supports the child emotionally but also affects the treatment positively. In addition, due to aspects of immature physiology and cognition during early childhood, family members play an important role in maintaining their child’s health and developing their behavior [1].
Family members influence the physical and emotional health of their children. Hence, involving them in planning the care and treatment services and increasing their power and responsibilities in the care enhances the effectiveness of the treatment. For this reason, children with chronic diseases receive care at home rather than at health institutions. Moreover, since these children have to live with the disease for life, they and their family members should have sufficient knowledge regarding the care and treatment of the disease. Therefore, children and families should be involved in both the health and disease processes in family-centered care (FCC) [2,3].
Studies have shown that FCC practices have many benefits, such as family members could obtain additional information regarding their child’s medical condition and care, information-sharing between healthcare professionals and the families, and decreased parent and patient anxiety levels [4-6]. Therefore, pediatric nurses’ cooperation with family members in determining the needs of the child and establishing communication is important, particularly during sickness and hospitalization. Normal developmental crises, which affect the child at different ages, manage the process and determine the support systems that will empower the child to cope with the sickness effectively in the hospital environment. In addition, pediatric nurses should simultaneously evaluate the child and the family, which is part of a holistic approach, when caring for a healthy or sick child [7,8].
According to literature reviews, the FCC model has been actively implemented in countries such as the United States, England, and Canada, and this approach has shaped healthcare policies (9-11]. This care model has been implemented in intensive care units (ICUs) and emergency clinics, with necessary settings made and conditions created to enable families to stay with their children for 24 h. [12]. According to Ahmann and Johnson (2001), FCC in hospitals is important in accelerating the child’s recovery process. Studies have reported that parents encouraged care based on FCC practices [13-16].
Dur et al. (2016) found that practices performed by mothers when caring for their children were mostly aimed at eliminating the need for nutrition and hygiene. Some nurses reported that families should not be involved when performing painful procedures on their children [17-19]. Nonetheless, nurses who work very closely with children and their families in the hospital have major responsibilities in improving FCC [19].
Studies conducted in Turkey reported that nurses did not inform the mothers regarding the care of their children and that the nurses were unavailable [19,20]. The examination of FCC in Turkey indicated a lack of regulation regarding family and children in hospitals and clinical settings, with every hospital following different practices. In some hospitals, children were not allowed to see their parents, except during visiting hours. To our knowledge, in Turkish hospitals where children are allowed to be with their families throughout the day, there are no studies conducted regarding parental involvement in treatment and care decisions, whether parents are informed about the status of their children, and whether FCC is at the desired level [20].
AIM OF THE STUDY
This study aimed to investigate the effect of FCC training on the attitude of pediatric nurses towards the FCC approach.
RESEARCH HYPOTHESES
The hypotheses of the research were the following:
H0: Training nurses working in pediatric clinics in FCC does not improve their care attitude. H1: Training nurses working in pediatric clinics in FCC improves their care attitude.
MATERIALS AND METHODS
Study design and setting
The study employed the pretest-posttest quasi-experimental and prospective design. A non- randomized trial was conducted in this research, adhering to the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) Statement Checklist.
The study was conducted at the neonatal ICU (NICU) and pediatric ICU (PICU) of a training and research hospital in Erzurum, Turkey between January 15 and April 15, 2018. The research was conducted face-to-face with nurses.
The pretest and posttest data of the control group were obtained between January 15 and February 15, 2018; the data of experimental group were collected between February 16 and April 15, 2018. Nurses’ training was conducted between February and April 2018.
These units were selected because it had a high number of beds; and these units had similar workloads, included a mother's hotel for long-term stays and were places where family-centered care practices are most needed.
Population and sample of the study
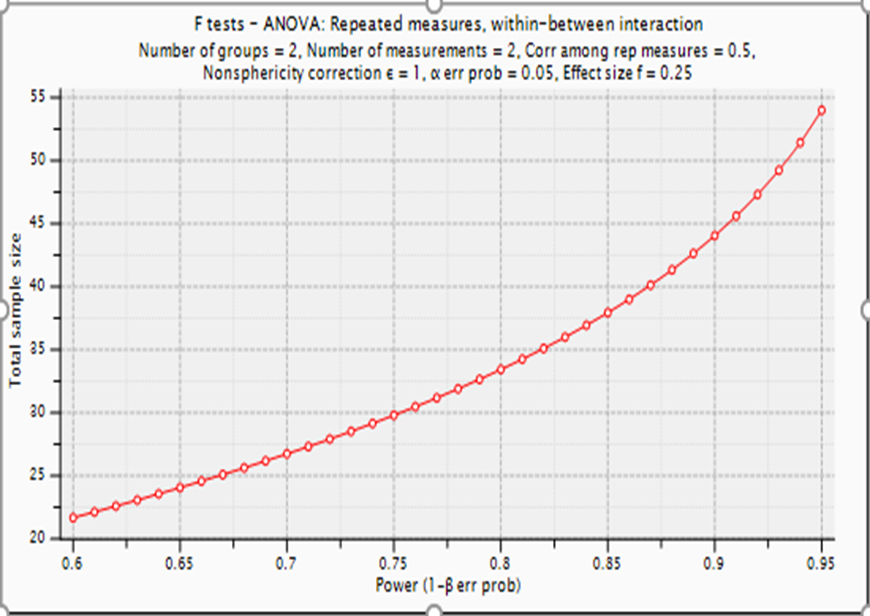
The population of the study comprised nurses who worked in PICU (N=31) and in NICU (N=35) of the hospital where the research was conducted. This of the 66 nurses, 33 were selected for the control group and 33 for the experimental group by simple random sampling method. Statistical power analysis using G*Power 3.1 was performed to determine the sample size. The analysis indicated that at least 54 nurses were needed at a significance level of 5% and an effect size of 0.25 to exceed 95% value. (df = 52; F = 4.027).
Of 66 nurses, 63 were included in the data collection process conducted between January 15 and April 15, 2018. One nurse was on leave, and two nurses did not agree to participate in the study. The study was completed with 63 nurses, including 30 in the experimental group and 33 in the control group. This study had a coverage rate of 95.4%.
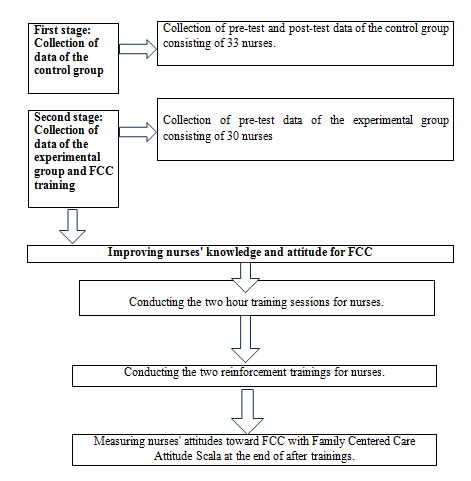
Inclusion criteria for nurses were volunteering to participate, working in pediatric intensive care and neonatal intensive care units for at least six months and participating in the FCC training conducted within the scope of the research. The objectives of the research were explained to the nurses who met these criteria, and written consent was obtained from the nurses who volunteered to participate in the study. Exclusion criteria for nurses were withdrawing from the research at any time and not attending any of the FCC training sessions conducted as part of the research. The data were collected by the researcher (Figure 1).
Figure 1. Power Analysis Diagram.
Data collection tools
Data were obtained using the descriptive characteristics form and the Family Centered Care Attitude Scale (FCCAS) developed by the researchers. An educational booklet and power point presentations for the education of nurses were used in the research.
Descriptive Characteristics Form: This form consisted of 10 questions regarding the nurses’ personal and professional characteristics: gender, age, marital status, family type, income status, educational status, unit where the nurses worked, duration of professional experience, number of patients per nurse, and their knowledge regarding FCC. This form was filled out during the interview after the nurses had agreed to participate in the study.
Family Centered Care Attitude Scale: FCCAS is a new measurement tool which was developed by Kara and Güdücü Tüfekci (2018) to evaluate the attitude of nurses working in pediatric clinics or nurses providing care to pediatric patients regarding FCC. The scale consisted of 58 five-point Likert-type items. Nurses explained their agreement or disagreements related to FCC attitudes and were rated from 1 to 5 (5 = Strongly Agree, 4 = Agree, 3 = Undecided, 2 = Disagree, 1 = Strongly Disagree). The scale has no reverse item, and it has two subscales: Contribution of Family-Centered Care (covers 1–28 items) and Family and Child Participation in Care (covers 29–58 items). Three scores were calculated: two subscales and overall attitude towards FCC. When determining the factors and measuring the general attitude scores, the value of the items was added and divided by the number of items (arithmetic mean). The subscales and total attitude score ranged from 1 to 5. An increase in the total score of the scale and the scores obtained from the subscales indicated a positive attitude of the nurses towards the contribution and necessity of FCC. The 4-point width of the scale score was divided into 5 equal parts (4/5 = 0.8): 1.00–1.79 points = very low level, 1.80–2.59 points = low level, 2.60–3.39 points = medium level, 3.40–4.19 points = high level, and 4.20–5.00 points = very high level.
The alpha coefficient of FCCAS, Contribution of the Family-Centered Care, and Family and Child Participation in Care was .982, .967, and .972, respectively [21].
Data collection process
The data collection process consists of two stages.
First stage: Collection of data of the control group
The study began with the control group; however, during the data collection process, nurses in the experimental group received the training, whereas nurses in the control group did not receive the training. Group studies were conducted at different time intervals to avoid any ethical issues, as there was a possible interaction between the nurses of both groups that could reveal the educational intervention.
Pre-test data of the control group started to be collected on January 15, and post-test data was completed on February 15. Descriptive characteristics form and family centered care attitude scale were used to collect the pretest data of control group. The posttest data was collected with only family centered care attitude scale.
Second stage: Collection of data of the experimental group and FCC training
Pretest data of the experimental group was collected on February 16, 2018. The pretest data of experimental group was obtained with descriptive characteristics form and family centered care attitude scale.
The nurses in the experimental group were divided into three groups of 10 people and each nurse was provided with an educational booklet to use during practice. Each group of nurses received two hours of training. The training segmented into three sessions of roughly 40 min each. The first session introduced the definition, fundamental principles, and underlying concepts of FCC. The second session scrutinized the impacts of FCC on families, children, and healthcare professionals. In the third session, nurses were informed about family-centered care practices. Nurses’ questions were answered during the trainings. The first FCC training of the experimental group was completed in February, 2018. Following the completion of the first FCC training, the evaluation of the experimental group was conducted using the FCCAS.
The two reinforcement training sessions were conducted to the experimental group in March and April. At the end of two reinforcement trainings, nurses' attitudes towards to family centered care with family centered care attitude scala were re-examined; the posttest data of the experimental group was completed on April 15, 2018 (Figure 2).
Figure 2. Data Collection and FCC trainings.
Content of family-centered care education
The aim of training was improving nurses knowledge, skills, and attitudes in order to increase parental involvement in care. The training content was created within the framework of the basic components current literature [22-26]. The training content, booklet and PowerPoint presentation used in the training were submitted to the expert opinion of five faculty members who have conducted studies on FCC. The training content and presentations were revised based on the feedback received. The FCC training focused on the definition of FCC and its basic concepts, goals, principles, and effects on the family, child, and healthcare team members.
Analysis and evaluation of the data
Descriptive characteristics form and family centered care attitude scale were used to collect the pretest data, and only family centered care attitude scale was used to collect the posttest data of both groups. There were no similarities between the nurses in both groups in terms of age group, gender, family type, and knowledge regarding FCC; thus, a similarity test could not be performed for these variables.
Statistical Package for Social Sciences for Windows 22.0 program and AMOS 21 program were used to analyze the data. Percentage and mean were used for determining the characteristics of the nurses. Chi-square analysis was used for evaluating intergroup similarities. Analysis of variance was used for determining levels of FCC according to its characteristics.
Ethical matters
The study protocol was approved by the ethics committee of Erzurum Atatürk University Faculty of Health Sciences (date: 09/01/2017 and number: 2016/12/06). Written approvals were obtained from the institutions where the study was conducted. Nurses were informed regarding the purpose and application method of the study, and verbal and written consent was obtained. Ethical principles including “Protection of Privacy and Confidentiality” were fulfilled by stating that the information obtained for this research would be kept confidential and not be used anywhere else. “Respect for Autonomy” principle was fulfilled by taking those who voluntarily participated in the study. Nurses were informed that they could withdraw from the study at any time.
RESULTS
In the experimental group, the average age of the nurses was 25.03 ± 4.45 years, 76.7% were female, 66.7% were single, 80% had equal income and expense, all lived in a nuclear family, 20% held an associate’s degree, 76.7% had 6–10 years of professional experience, 50% worked in NICU, 56.7% provided care to ≤3 patients, and all had limited knowledge regarding FCC (Table 1).
Table 1. Descriptive characteristics of the nurses (N = 63)
|
Characteristics |
Experimental Group |
Control Group |
Total |
Test and Score |
|||
|
N |
% |
N |
% |
N |
% |
||
|
Marital Status* |
|
|
|
|
|
|
|
|
Married |
10 |
33.3 |
12 |
36.4 |
22 |
34.9 |
χ2 = .063 p = 1.00 |
|
Single |
20 |
66.7 |
21 |
63.6 |
41 |
65.1 |
|
|
Income Status*+ |
|
|
|
|
|
|
|
|
Income less than expense |
6 |
20.0 |
16 |
48.5 |
22 |
34.9 |
χ2 = 5.610 p = .033 |
|
Income equal to expense |
24 |
80.0 |
17 |
51.5 |
41 |
65.1 |
|
|
Graduation Degree ** |
|
|
|
|
|
|
|
|
Vocational School of Health |
12 |
40.0 |
4 |
12.1 |
16 |
25.3 |
χ2 = 7.966 p = .019 |
|
Associate Degree |
6 |
20.0 |
5 |
15.2 |
11 |
17.4 |
|
|
Bachelor Degree |
12 |
40.0 |
24 |
72.7 |
36 |
57.1 |
|
|
Professional Experience* |
|
|
|
|
|
|
|
|
1–5 Years |
23 |
76.7 |
28 |
54.9 |
51 |
84.8 |
χ2 = .682 p = .525 |
|
6–10 Years |
7 |
23.3 |
5 |
41.7 |
12 |
15.2 |
|
|
Unit * |
|
|
|
|
|
|
|
|
Neonatal Intensive Care |
15 |
50.0 |
18 |
54.5 |
33 |
52.3 |
χ2 = .130 p = .803 |
|
Pediatric Intensive Care |
15 |
50.0 |
15 |
45.5 |
30 |
47.6 |
|
|
Number of Patients per Nurse ** |
|
|
|
|
|
||
|
3 patients or less |
17 |
56.7 |
14 |
42.4 |
31 |
49.2 |
χ2 = 1.275 p = .317 |
|
4–6 |
13 |
43.3 |
19 |
57.6 |
32 |
50.8 |
|
|
Age Average (X ± SD) |
25.03 ± 4.45 |
24.96 ± 2.51 |
25.00 ± 3.54 |
t = .071 p = .944 |
|||
*Fisher’s Exact Test, **Pearson’s Chi-Square Test, + There was no participant who had an income more than the expense.
In the control group, the average age of the nurses was 24.96 ± 2.51 years, all were female, 63.6% were single, 65.1% had equal income and expense, all lived in a nuclear family, 57.1% held a bachelor’s degree, 84.8% had 1–5 years of professional experience, 52.3% worked in NICU, 50.8% provided care to 4–6 patients, and 39.4% had knowledge regarding FCC. Table 1 shows that the average age, marital status, family type, professional experience of the nurses, units where the nurses work, and number of patients per nurse were similar between both groups (p ˃ .05).
The mean score of the pretest FCCAS of all the nurses participating in the experimental stage was 4.13 ± .44, the mean score of the Contribution of Family-Centered Care subscale was 4.15 ± .48, and the mean score of Family and Child Participation in Care subscale was 4.11 ± .48 (Table 2).
Table 2. Family-centered care attitude scale scores of the nurses (N = 63)
|
Scale |
Items |
Number of Items |
Scale |
Received |
Received |
|
Min–Max |
Min–Max |
X ± SD |
|||
|
Contribution of Family-Centered Care |
1–28 |
28 |
1–5 |
3.18–5 |
4.15 ± .48 |
|
Family and Child Participation in Care |
29–58 |
30 |
1–5 |
3.00–5 |
4.11 ± .48 |
|
Family-Centered Care Attitude Total |
1–58 |
58 |
1–5 |
3.09–5 |
4.13 ± .44 |
In the intergroup comparison, we found a significant difference between the mean scores of the nurses in pretest FCCAS. The control group had higher scores (p < .05) than the experimental group; however, the mean scores of the posttest FCCAS increased significantly in the experimental group (p < .001) (Table 3). Furthermore, we found a significant difference between the mean scores of the nurses in the pretest Contribution of Family-Centered Care subscale. The control group had higher scores (p < .05) than the experimental group; however, the mean scores of the posttest Contribution of Family-Centered Care subscale increased significantly in the experimental group (p < .001) (Table 3). In addition, there was a significant difference between the mean scores of the nurses in the pretest Family and Child Participation in Care subscale. The control group had higher scores (p < .05) than the experimental group; however, the mean scores of the posttest Family and Child Participation in Care subscale increased significantly in the experimental group (p < .001) (Table 3).
In the intragroup comparison, we found that the mean scores of the nurses in the experimental group increased significantly in posttest FCCAS, Contribution of Family-Centered Care subscale, and Family and Child Participation in Care subscale (p < .001) (Table 3).
Table 3. Comparison of intergroup and intragroup pretest–posttest mean scores of the nurses in terms of family-centered care attitude scale and its subscales (N = 63)
|
Family-Centered Care Attitude Scale |
Experimental Group (N = 30) |
Control Group (N = 33) |
t/p* |
|||
|
X̄± SD |
Min–Max |
X̄± SD |
Min–Max. |
|||
|
SCALE
TOPLA |
Pretest |
3.98 ± .42 |
3.21–4.81 |
4.26 ± .42 |
3.09–5.00 |
t = 2.627 p = .011 |
|
Posttest |
4.78 ± .26 |
4.24–5.00 |
4.29 ± .31 |
3.52–5.00 |
t = 6.644 p = .000 |
|
|
Test and s |
z = -4.783 p = .000 |
z = -.657 p = .511 |
|
|||
|
SUBSCALES |
Contribution of Family-Centered Care |
|
|
|
||
|
Pretest |
4.01 ± .49 |
3.32–4.93 |
4.27 ± .44 |
3.18–5.00 |
t = 2.184 p = .033 |
|
|
Posttest |
4.76 ± .28 |
4.04–5.00 |
4.32 ± .38 |
3.50–5.00 |
t = 5.150 p = .000 |
|
|
Test and s |
z = -4.762 p = .000 |
z = -.353 p = .724 |
|
|||
|
Family and Child Participation in Care |
|
|
|
|||
|
Pretest |
3.95 ± .47 |
3.10–4.90 |
4.26 ± .46 |
3.00–5.00 |
t = 2.582 p = .012 |
|
|
Posttest |
4.80 ± .28 |
3.97–5.00 |
4.26 ± .34 |
3.23–5.00 |
t = 6.601 p = .000 |
|
|
Test and s |
z = -4.704 p = .000 |
z = -.112 p = .911 |
|
|||
DISCUSSION
Studies have reported the necessity of maintaining the mother–child relationship when a child is hospitalized. FCC has become one of the basic principles of pediatric nursing, based on which care practices have been developed [27-29].
In this study, we discussed the outcomes of FCC training provided to nurses working in pediatric clinics to improve their attitude towards FCC and we confirmed hypothesis H1, along with the results of the survey studies since no study result included the scale evaluations. In addition, since there were no similarities in age group, gender, family type, and knowledge regarding FCC between the nurses in both groups, a similarity test could not be performed for these variables. There were no similarities in income level and graduation degree (p < .05) between both groups. We considered these situations as the limitations of the study. At this stage, we only considered nurses whose average age, marital status, family type, professional experience, unit worked, and number of patients per nurse were similar (p ˃ .05) (Table 1).
The participants’ FCCAS mean score before the intervention was 4.13 ± .44, mean score for Contribution of Family-Centered Care subscale was 4.15 ± .48, and mean score of Family and Child Participation in Care subscale was 4.11 ± .48 (Table 2). According to the literature on assessment and evaluation, the 4-point width of the scale score was divided into 5 equal parts (4/5 = .8): scores 1.00–1.79 = very low level, 1.80–2.59 = low level, 2.60–3.39 = medium level, 3.40–4.19 = high level, and 4.20–5.00 = very high level [30]. In line with this literature, we concluded that nurses included in this study had knowledge regarding FCC, and their attitudes regarding FCC, Contribution of Family-Centered Care subscale, and Family and Child Participation in Care subscale were at a high level.
Studies conducted on FCC practices in Turkey reported that nurses did not perceive these practices correctly, the practices were not at the desired level, and giving most of the child’s care and treatment practices to the mother’s responsibility was not FCC [25,31]. FCC is the integration of family into delivering care to a sick child [28]. It is a care approach that best meets the needs and expectations of children and parents in the hospital [32]. Therefore, to ensure that the child received the best level and quality of care [33], nurses should partner with family members (15) to formulate a treatment plan and evaluate and implement them accordingly [34].
A study suggested that parents encouraged care for their children based on these principles [35]. Studies have shown that children with parents involved in care had fewer behavior problems [36], reduced need for analgesics in the ICU, and faster recovery time (32]. In addition, infants had a positive pain experience and fewer stress findings [33]. This form of care also had positive effects on infants receiving phototherapy (39). Despite some of the benefits, the FCC model is still not implemented due to the lack of knowledge, which is a critical deficiency (34]. Providing FCC training to all nurses involved in providing care to pediatric patients is imperative [20].
In the pretest intergroup comparison, nurses in the control group had significantly higher FCC attitudes (p < .05) than the experimental group. In the posttest intergroup comparison, a significant improvement in nurses’ attitude was observed in the experimental group (p < .001). In addition, attitudes of the nurses in the control group were significantly higher in the Contribution of Family-Centered Care and Family and Child Participation in the Care subscales of FCCAS (p < .05). In the posttest intergroup comparison, a significant increase was determined in nurses’ attitudes in the experimental group (p < .001). Likewise, in the intragroup comparison, a significant increase was observed in nurses’ attitudes in the experimental group regarding FCC, its contribution, and family and child participation in care in the post-test (p < .001, Table 3). Our finding that the attitude of the control group in pretest and attitude of the experimental group in posttest were significantly high was important, as this indicates that FCC training is highly effective in developing attitudes. The significantly high level of attitudes of the control in pre-test reinforced the research results.
In similar experimental studies conducted without scale evaluation, it was observed that FCC training resulted in nurses and physicians developing positive attitudes towards the child and family [40], increased knowledge and understanding regarding FCC among nurses, cooperation and effective communication between parents and nurses, reduced anxiety among children and parents, and nurses gaining autonomy [39,40]. In addition, nurses had more empathic communication with the family and the child, physicians devoted more time to their patients, and provided more information to them [40]. These results support the findings of the present study regarding changes in the attitude of healthcare professionals who underwent FCC training, particularly pediatric nurses. The results of the intergroup and intragroup comparisons of the experimental group supported hypothesis H1.
PRACTICAL IMPLICATIONS
Family-centered care is a care approach that meets the best the requirements and expectations of the child and family in an hospital environment. Pediatric nurses play a key role in enabling hospital care services to become family-centered. Therefore, pediatric nurses need to embrace and extend the family-centered care approach to increase the quality of care and enhance the patient satisfaction.
For the improvement of family centered care practices, it is necessary to eliminate the lack of information about the practices and support and conduct high-quality research that can provide guidance.Nurses working in pediatric clinics can be educated about care in developing family-centered care attitude. it is essential that nurses are supported by all related managers and multidisciplinary team members during FCC implementations.
LIMITATIONS OF THE RESEARCH
The limitations of the study were that the nurses in the experimental and control groups could not form similar groups in terms of age group, gender and family type characteristics, and they were not similar in terms of income status and graduation degree. Conducting this study within one hospital may be a limitation. The sample size of the current study had been small. Research of this kind, it does require caution when generalizing the results. The results at this stage can be generalized to nurses with similar average age, marital status, and professional experience. The impact of FCC trainings may vary according to the differences in each country and hospital conditions.
CONCLUSIONS
In this study, in the experimental group, FCC training significantly increased the nurses’ attitude towards FCC, Contribution of Family-Centered Care, and Family and Child Participation in Care as compared to nurses in the control group. In order to maintain positive attitudes toward family-centred care and practise FCC at an optimal level, pediatric nurses should receive continued training. Therefore, we recommend providing FCC training to nurses working in pediatric clinics to improve their attitude towards FCC.
ACKNOWLEDGMENTS
The authors thank the pediatric nurses who are in Erzurum for participating in this study.
CONTRIBUTORS
Concept: A.K., F.G.T., Design: A.K., F.G.T., Data Collection or Processing: A.K., F.G.T., Analysis or Interpretation: A.K., F.G.T., Literature Search: A.K., F.G.T., Writing: A.K., F.G.T.
CONFLICT OF INTEREST
No conflict of interest was declared by the authors.
FINANCIAL DISCLOSURE
The authors declared that this study received no financial support.
REFERENCES
- Altıparmak D, Taş Arslan F. (2016). Aile Merkezli Bakım Ölçeği’nin Türkçe’ye uyarlanması geçerlik ve güvenirlik çalışması. J Pediatr Res. 3:97-103.
- Ocakçı AF. (2006). Aile Merkezli Hemşirelik Bakımı: Çocuğun Aile Merkezli Bakımı, 1. Baskı. Zonguldak, Dökel Matbaası. 2006: 8-27.
- Çavuşoğlu H. (2013). Çocuk Sağlığı Hemşireliği, 11. Baskı. Ankara, Cilt 1, Sistem Ofset. 2013:5.
- Dennis C, Baxter P, Ploeg J, Blatz S. (2016). Models of partnership within family-centred care in the acute paediatric setting: a discussion paper. J Adv Nurs. 73(2):361-374.
- Feeg V, Paraszczuk A, Çavuşoğlu H, Shields L, Pars H, Al Mamun A. (2016). How is family centered care perceived by healthcare providers from different countries? An international comparison study. J Pediatr Nurs. 31(3):267-276.
- Harrison TM. (2010). Family-centered pediatric nursing care: State of the science. J Pediatr Nurs. 25(5):335-343.
- İşler A, Conk Z. (2006). Family-centred care in paediatrics. Ege Paediatrics Bulletin. 13:187-193.
- Çavuşoğlu H. (2018). Pediatri kliniklerinde aile merkezli bakımda yaşanan sorunlar ve yeni yaklaşımlar. Türkiye Klinikleri J Nurs. 10(4):344-353.
- Byers J, Lowman L, Francis J, Kaigle L, Lutz N, Waddell T. (2006). A quasi-experimental trial on individualized, developmentally supportive family-centered care. J Obstet Gynecol Neonatal Nurs. 35(1):105-115.
- Mantha S, Davies B, Moyer A, Crowe K. (2008). Providing responsive nursing care to new mothers with high and low confidence. Am J Matern-Chil. 33(5):307-314.
- Shields L. (2015). What is “family-centred care”? European Journal for Person Centered Healthcare. 3(2):139-144.
- Tosun A, Tüfekçi FG. (2015). The examination of family centered care practices in pediatric clinics. Journal of Anatolia Nursing and Health Sciences. 18(2):131-139.
- Ahmann E, Johnson BH. (2001). New guidance materials promote family-centered change in health care institutions. Pediatr Nurs. 27(2):173-175.
- Shields L, Nixon J. (2004). Hospital care of children in four countries. J Adv Nurs. 45(5):475-486.
- Ward K. (2001). Perceived needs of parents of critically ill infants in a neonatal intensive care unit (NICU). Pediatr Nurs. 27(3):281-286.
- Magnusson DM, Mistry KB. (2017). Racial and ethnic disparities in unmet need for pediatric therapy services: the role of family-centered care. Acad Pediatr. 17(1):27-33.
- Dur Ş, Gözen D, Bilgin M. (2016). Devlet ve özel hastanelerdeki hemşirelerin aile merkezli bakıma ilişkin tutum ve davranışları. J Curr Pediatr. 14:1-9.
- MacKay LJ, Gregory D. (2011). Exploring family-centered care among pediatric oncology nurses. J Pediatr Oncol Nurs. 28(1):43-52.
- Tüfekci FG, Erci B. (2007). The opinion of children, parents and health staff about parental presence during painful procedures. Journal of Anatolia Nursing and Health Sciences. 10(4):52-62.
- Oktay H, Çavuşoğlu H. (2009). Examination of the care given in a university hospital in terms of family-centred care and determining the opinions of the mothers. H.U. Faculty of Health Sciences, Journal of Nursing. 16:11-24.
- Kara A, Güdücü Tüfekci, F. (2018). The impact of family-centred care training on knowledge and attitudes of paediatric nurses [Unpublished doctoral dissertation]. Atatürk University, Institute of Health Sciences.
- Aldem M, Geçkil E. (2019). The concept and principles of family-centered care in pediatric nursing. In E. Gekil (Ed.). Family centered Care in Pediatric Nursing. 1st ed. Ankara: Turkey Clinics. p. 1-4.
- Bozkurt G, Duzkaya DS, Oren B. (2021). Opinions of intensive care nurses about family-centered care in Turkey. International Journal of Caring Sciences. 14(1):45-53.
- Dall’Oglio I, DiFuria M, Tiozzo E, Gawronski O, Biagioli V, DiCiommo V, et al. (2018). Practices and perceptions of family centered care among healthcare providers: A cross-sectional study in a pediatric hospital. J Pediatr Nurs. 43:e18-e25.
- Öztürk C, Ayar D. (2019). Reflections of family-centered care in pediatrics on children, families and nurses. In E. Gekil (Ed.), Family centered Care in Pediatric Nursing. 1st ed. Ankara: Turkey Clinics. pp. 12-17.
- Yoo SY, Cho H. (2020). Exploring the influences of nurses’ partnership with parents, attitude to families’ importance in nursing care, and professional self- efficacy on quality of pediatric nursing care: A path model. Int J Environ Res Public Health. 17(15):5452.
- Brown K, Mace SE, Dietrich AM, Knazik S, Schamban NE. (2008). Patient and family-centred care for pediatric patients in the emergency department. CJEM. 10(1):38-43.
- Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. (2007). Impact of a family-centered care initiative on NICU care, staff and families. J Perinatol. 27(Suppl 2):S32-S37.
- Petersen MF, Cohen J, Parsons V. (2004). Family centered care: Do we practice what we preach. J Obstet Gynecol Neonatal Nurs. 33(4):421-427.
- Ryan E, Steinmiller E. (2004). Modeling family- centered pediatric nursing care: strategies for shift report. J Spec Pediatr Nurs. 9(4):123-128.
- Boztepe H. (2009). Family-centred care in paediatric nursing. Türkiye Klinikleri J Nurs. 1(2):88-93.
- Neal A, Frost M, Kuhn J, Green A, Gance-Cleveland B, Kersten R. (2007). Family centered care within an infant-toddler unit. Pediatr Nurs. 33(6):481-485.
- Kitchen BE. (2005). Family-centered care: A case study. J Spec Pediatr Nurs. 10(2):93-97.
- Frost M, Green A, Gance-Cleveland B, Kersten R, Irby C. (2010). Improving family-centered care through research. J Pediatr Nurs. 25(2):144-147.
- Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. (2006). Reducing premature ınfants' length of stay and ımproving parents' mental health outcomes with the creating opportunities for parent empowerment (COPE) Neonatal intensive care ünit program: A randomized, controlled trial. Pediatrics. 118(5):e1414-e1427.
- Kamerling SN, Lawler LC, Lynch M, Schwartz AJ. (2008). Family centered care ın the pediatric post anesthesia care unit: Changing practice to promote parental visitation. J Perianesth Nurs. 23(1):5-16.
- Westrup B. (200). Newborn ındividualized developmental care and assessment program (NIDCAP)- Family-centered developmentally supportive care. Early Hum Dev. 83(7):443-449.
- Szucs KA, Rosenman MB. (2013). Family-centered, evidence-based phototherapy delivery. Pediatrics. 131(6):e1982-e1985.
- Günay U, Polat S. (2017). Pediatrik onkoloji kliniğinde verilen aile merkezli bakım eğitiminin değerlendirilmesi: Hekim ve hemşire görüşleri. Bozok Tıp Derg. 7:12-21.
- Shields L, Zhou H, Pratt J, Taylor M, Hunter J, Pascoe E. (2012). Family-centred care for hospitalised children aged 0–12 years. Cochrane Database Syst Rev. 10:CD004811.