Previous Issues Volume 8, Issue 3 - 2024
Revolutionizing Rehabilitation: Prosthodontic Management of Distal Extension Using Cobalt-Chromium Cast Partial Dentures: A Case Report
Arpit Sikri1,*, Vaishali Kalra2, Jyotsana Sikri3
1Associate Professor & Post Graduate Teacher, Department of Prosthodontics, Crown & Bridge and Oral Implantology, Bhojia Dental College & Hospital, Budh (Baddi), India
2Post Graduate (PG) Student, Department of Prosthodontics, Crown & Bridge and Oral Implantology, Bhojia Dental College & Hospital, Budh (Baddi), India
3Associate Professor & Post Graduate Teacher, Department of Conservative Dentistry & Endodontics, Bhojia Dental College & Hospital, Budh (Baddi), India
*Corresponding Author: Dr. Arpit Sikri, Associate Professor & Post Graduate Teacher, Department of Prosthodontics, Crown & Bridge and Oral Implantology, Bhojia Dental College & Hospital, Budh (Baddi), Teh. Baddi, Distt. Solan, Himachal Pradesh, India, Phone: +91-7011836989, E-mail: [email protected]
Received Date: October 10, 2024
Published Date: November 07, 2024
Citation: Sikri A, et al. (2024). Revolutionizing Rehabilitation: Prosthodontic Management of Distal Extension Using Cobalt-Chromium Cast Partial Dentures: A Case Report. Mathews J Dentistry. 8(3):54.
Copyrights: Sikri A, et al. © (2024).
ABSTRACT
The primary objective of prosthodontic rehabilitation is to restore a patient's form, function, aesthetics, and phonetics. Various treatment options are available for rehabilitating a partially edentulous arch, including removable partial dentures (RPD) or removable dental prostheses (RDP), overdentures, conventional fixed partial dentures or fixed dental prostheses (FDP), and implant-supported prostheses. Replacing a missing tooth necessitates a careful intraoral examination of the patient's current clinical condition. Additionally, it involves evaluating the associated risks, benefits, and costs of the chosen treatment option, followed by a detailed discussion with the patient. Replacing single or multiple missing teeth with removable partial dentures in distal extension scenarios presents significant challenges due to mucosal displacement caused by occlusal forces. Cast partial dentures (CPD) have recently emerged as a practical solution when fixed options are not viable, either due to the patient’s oral condition or financial constraints. The traditional laboratory procedures for fabricating CPD frameworks are complex, time-consuming, and demand high precision from the dental surgeon. However, modern digital technology has simplified these processes significantly. When edentulous areas are too extensive or numerous for fixed prostheses and cross-arch stabilization is needed, a cast partial denture (CPD) is the preferred option. The procedures for inserting, removing, and maintaining oral hygiene with a CPD are straightforward. However, designing a partial denture for distal extension cases requires considerable skill due to the variations in tooth and soft tissue, which can lead to non-axial loading. Effective management of forces relies on maintaining optimal tissue health, maximizing soft tissue coverage, using direct retainers properly, and positioning all components advantageously. In cases where cast partial dentures are not effective, flexible dentures may serve as an alternative. The present case report details the prosthetic rehabilitation of a partially edentulous patient using both maxillary and mandibular cast partial dentures (CPD) fabricated with Cobalt-Chromium. The article also aims to offer a comprehensive overview of this treatment approach through the case report.
Keywords: Bilateral Distal Extension Cases, Cast Partial Denture, Cross Arch Stabilization, Distal Extension, Financial Status, Removable Partial Denture, RPD Design, Surveying, Wax Pattern.
INTRODUCTION
Edentulism is a severe and often irreversible condition that significantly impacts oral health, particularly among the elderly, making it a global concern. For partially edentulous patients, effective prosthetic restoration is challenging due to the ongoing loss and deterioration of alveolar bone, adjacent teeth, and supporting structures [1]. Treatment options for these patients include interim removable partial dentures (RPD), definitive cast partial dentures (CPD), tooth-supported fixed partial dentures or fixed dental prostheses (FDP), and implant-supported prostheses, depending on the specific clinical situation [2].
A Removable Partial Denture (RPD) is a prosthesis that replaces some teeth in a partially edentulous arch and can be readily inserted and removed from the mouth by the patient (GPT 10) [3]. The primary goal of such a prosthesis is to preserve oral structures. Kennedy’s Class I and II removable partial dentures, which are not fully supported by teeth, present more complex challenges for successful oral rehabilitation [4]. Distal extension partial dentures are commonly fabricated using the altered cast impression technique, which helps to evenly distribute stress between soft and hard tissues, reduce the load on abutment teeth, minimize food impaction, and preserve the residual ridges, thereby enhancing patient satisfaction [5]. The free-end saddle of a partial denture may rotate gingivally under functional loading, potentially causing harm to the periodontium of the adjacent abutment tooth [6]. To address this, Kratochvil proposed a design incorporating a mesial occlusal rest, a proximal plate, and an I-bar to minimize such damage. Additionally, Krol introduced the RPI clasp design, which includes an I-bar, a proximal plate, and a mesial rest to reduce tooth surface coverage and lessen stress on the abutment tooth [7]
Removable Partial Dentures (RPDs) are widely accepted and cost-effective for patients with partially edentulous arches. Effective prosthetic rehabilitation of distal extension RPDs is essential for the long-term success and preservation of remaining natural teeth and their supporting structures [8]. Bilateral distal extension RPDs present challenges due to varying support levels between abutment teeth and residual ridges, making precise design crucial for maintaining natural teeth [9]. Clinical research indicates that acrylic removable prostheses can significantly damage the periodontium of abutment teeth compared to cast metal removable partial dentures [10]. Cast Partial Dentures (CPDs) provide superior retention, stability, comfort, and periodontal health for abutments, offering benefits such as precise, durable, and easy-to-clean metal bases.
In recent times, with the advent of technological advancements, digital dentistry—including digital surveying, designing, and 3D printing—has significantly improved the fabrication of CPDs [11]. However, not all clinical scenarios involving multiple missing teeth can be addressed with CPDs, necessitating careful selection of the most suitable prosthesis. Flexible dentures can serve as an alternative when CPDs are not effective, particularly in Kennedy’s Class I and II cases with distal extension [12].
The present manuscript reviews a case report on the prosthetic rehabilitation of a partially edentulous maxillary and mandibular arch using a Cobalt-Chromium CPD. It emphasizes improvements in retention, stability, support, aesthetics, and masticatory function. Moreover, the manuscript highlights the advantages of metal-based frameworks over acrylic ones and underscores the importance of selecting the most appropriate prosthesis for each patient.
Top of Form
CASE REPORT
Patient Information
A 60-year-old female visited the Department of Prosthodontics, Crown & Bridge, and Oral Implantology, seeking replacement for her missing upper and lower teeth, as she was unable to chew properly. She had undergone multiple extractions two years ago due to severely decayed posterior teeth in both arches.
Investigations Radiographic evaluation, including an OPG (Orthopantomogram) (Figure 1) and IOPA (Intraoral Periapical Radiograph) (Figure 2), revealed sufficient bone support around the remaining teeth, with no signs of periodontal or periapical issues.
Figure 1. Radiographic Investigation: OPG.
Figure 2. Radiographic Investigation: IOPA.
Extraoral Examination
The extraoral assessment showed no facial asymmetry or temporomandibular joint (TMJ) abnormalities. The patient's overall health appeared fair, and there were no significant findings in the lips, cheeks, tongue, floor of the mouth, palate, or TMJ.
Intraoral Examination
Intraorally, the patient presented with a dentition classified as Kennedy’s Class I in both the maxillary and mandibular arches. Specifically, the maxillary arch was Kennedy Class I, Modification 1, and the mandibular arch was Kennedy Class II, Modification 1 (Figures 3 & 4). The missing teeth included 13, 16, 17, 23, 24, 25, 26, 27, 36, 37, 44, 45, and 46, with carious lesions present on teeth 11 and 12. The remaining teeth were periodontally healthy and suitable to serve as abutments for a removable prosthesis. The previous partial dentures showed signs of fractures and multiple repairs, and the patient expressed dissatisfaction with their instability. The occlusion in both the maxillary and mandibular arches exhibited group function (Figures 5 & 6).
Figure 3. Intraoral Examination: Maxillary Arch.
Figure 4. Intraoral Examination: Mandibular Arch.
Figure 5. Examination of Occlusion (Molar Relation): Left Lateral View.
Figure 6. Examination of Occlusion (Molar Relation): Right Lateral View.
Treatment Options & Planning
Following complete oral prophylaxis, diagnostic impressions were made using irreversible hydrocolloid impression material (Zelgan 2002, Dentsply India Pvt. Ltd., Haryana, India) and poured into Type III dental stone (GypRock Stone, Rajkot, Gujarat, India). Several treatment options were considered, ranging from conventional removable partial dentures to implant-supported prostheses. However, implant-supported solutions were ruled out due to insufficient bone volume and financial constraints. Additionally, a fixed partial denture was not viable due to the absence of posterior abutments. After a thorough examination, and considering the patient's age, aesthetic, and functional needs, conventional cast partial dentures for both the maxillary and mandibular arches were deemed the most suitable option. The treatment plan was explained to the patient, who consented to proceed.
Treatment The patient was referred to the Periodontics and Conservative Dentistry & Endodontics departments for oral prophylaxis and restorative treatment of cervical abrasion lesions on teeth 25 and 44, as well as aesthetic restorations on tooth 22.
Proposed Mouth Preparations
Preparations included tooth reduction for guiding planes on teeth 15, 22, and 47, and rest seat preparations on teeth 11, 12, 21, 22 (palatal), 14 (distal), 15 (mesial), 33, 35 (mesial), 43, and 47 (mesial). Tooth preparation was performed on tooth 14, and a final impression was made for a PFM (porcelain-fused-to-metal) restoration (Figures 7 & 8), specifically a PFM crown on tooth 14 with a prepared rest seat.
Figure 7. PFM Restoration (Crown) with respect to 14 on the Cast.
Figure 8. PFM Restoration (Crown) with respect to 14 in Patient’s Mouth.
Procedure Diagnostic impressions (Figures 9 & 10) were made, followed by pouring the impressions to obtain diagnostic casts. After obtaining the diagnostic casts (Figure 11), a preliminary design for the removable partial denture was created. The casts were placed on a surveyor (Austenal Surveyor, Dentsply Sirona, Haryana, India) (Figure 12) for examination. Facebow transfer (Hanau™ Springbow, Whip Mix, Kentucky, USA) and interocclusal records were taken using a Hanau semi-adjustable articulator (Hanau™ Wide-Vue, Whip Mix, Kentucky, USA). An arbitrary design of the removable partial denture was created (Figure 13). Mouth preparations were completed, and final impressions of the mandibular arch were taken using the putty-wash technique with elastomeric impression material (Figure 14). Secondary casts were placed on a surveyor to finalize the cast framework design.
Figure 9. Diagnostic Impressions: Maxillary Arch.
Figure 10. Diagnostic Impressions: Mandibular Arch.
Figure 11. Diagnostic Casts.
Figure 12. Surveying the Cast Using a Surveyor.
Figure 13. Planned Design: Design of the Cast Partial Denture on the Maxillary and Mandibular Casts.
Figure 14. Final Impressions.
In the maxillary distal extension base, the retentive lattice configuration was extended to the hamular notch, and an antero-posterior palatal strap was selected as the major connector to provide support and rigidity. Cingulum rests were incorporated for teeth 13 and 23, and an I-bar direct retainer was used for enhanced retention. Mock rest seat and guide plane preparations were made on teeth 13 and 23 on the cast and carried out in the patient’s mouth. For the mandibular distal extension base, a double lingual bar was chosen as the major connector. The retentive lattice configuration was extended to two-thirds of the retromolar pad area. Border molding was completed using low-fusing green stick compound (Pinnacle Tracing Sticks, Dental Products of India, Mumbai, India), followed by final impressions using polyvinyl siloxane (Aquasil Soft Putty, Aquasil Light Body, Dentsply, Germany).
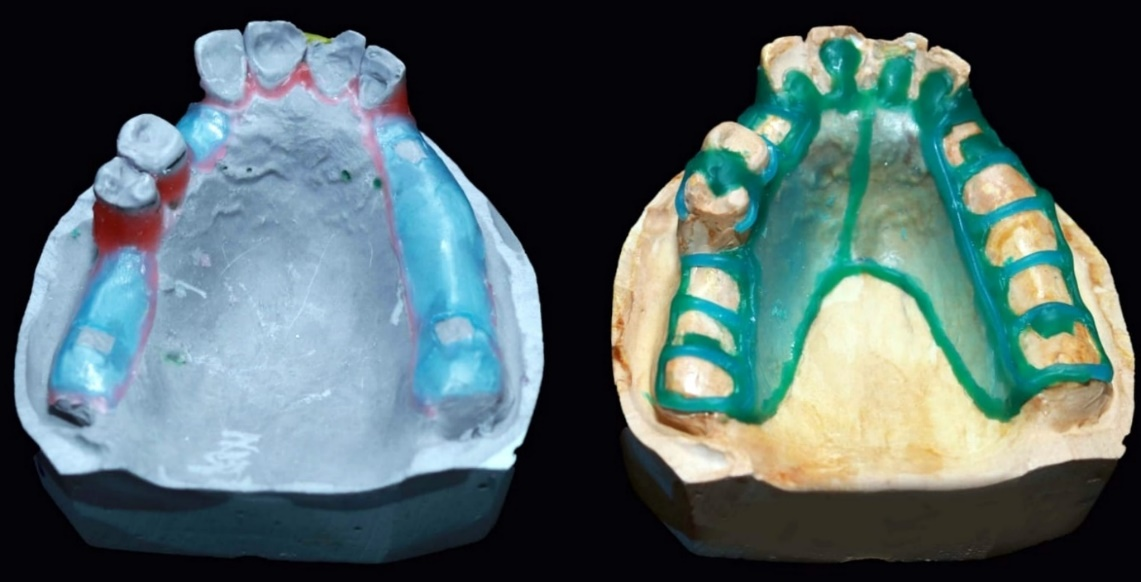
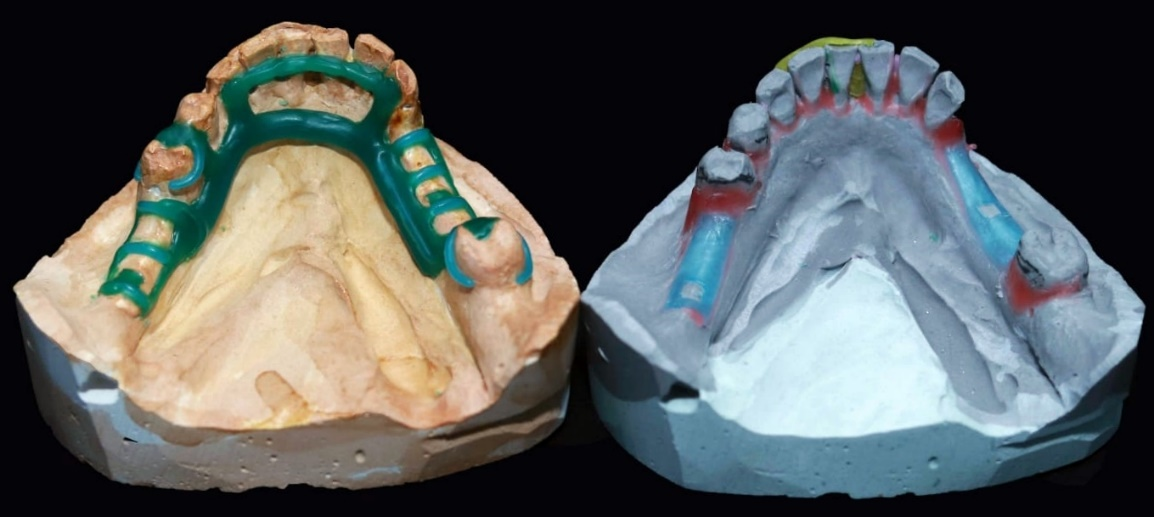
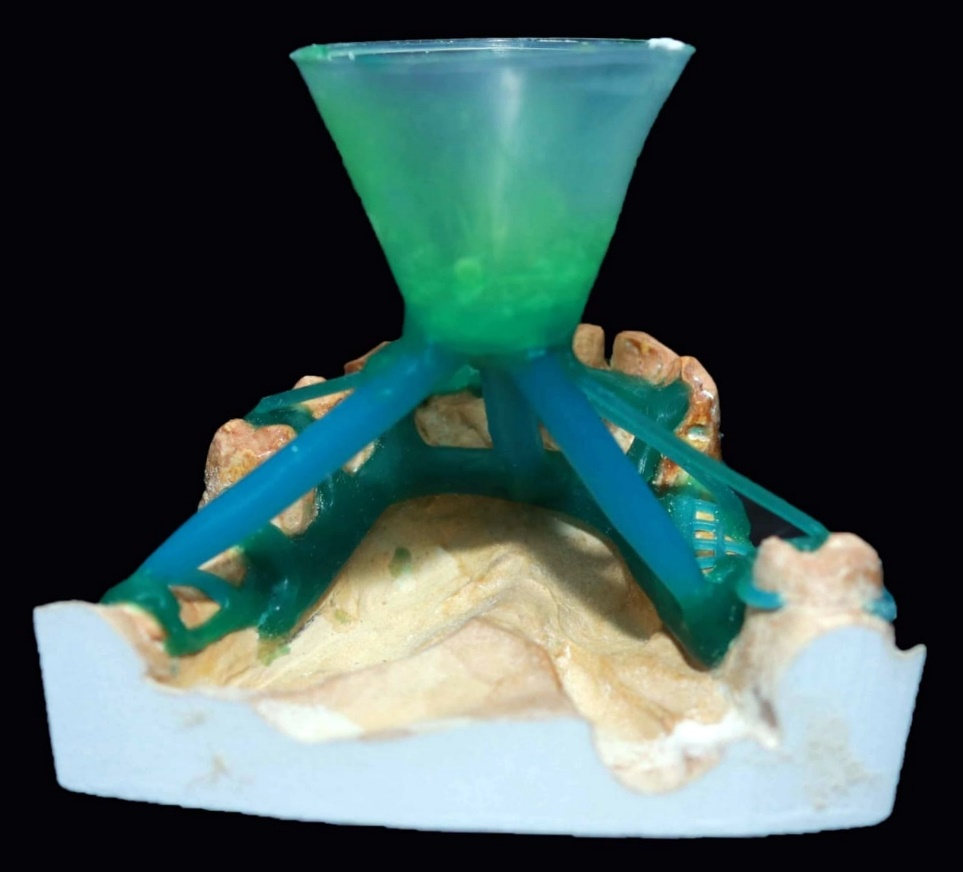
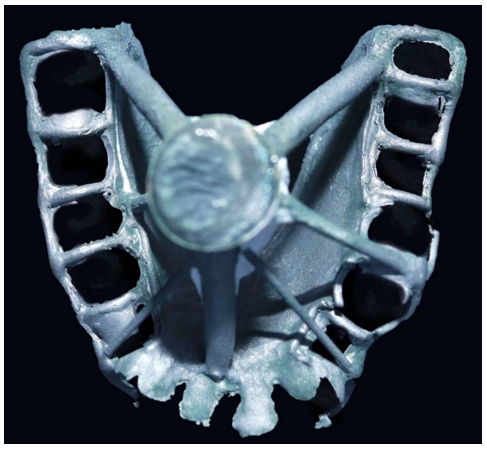
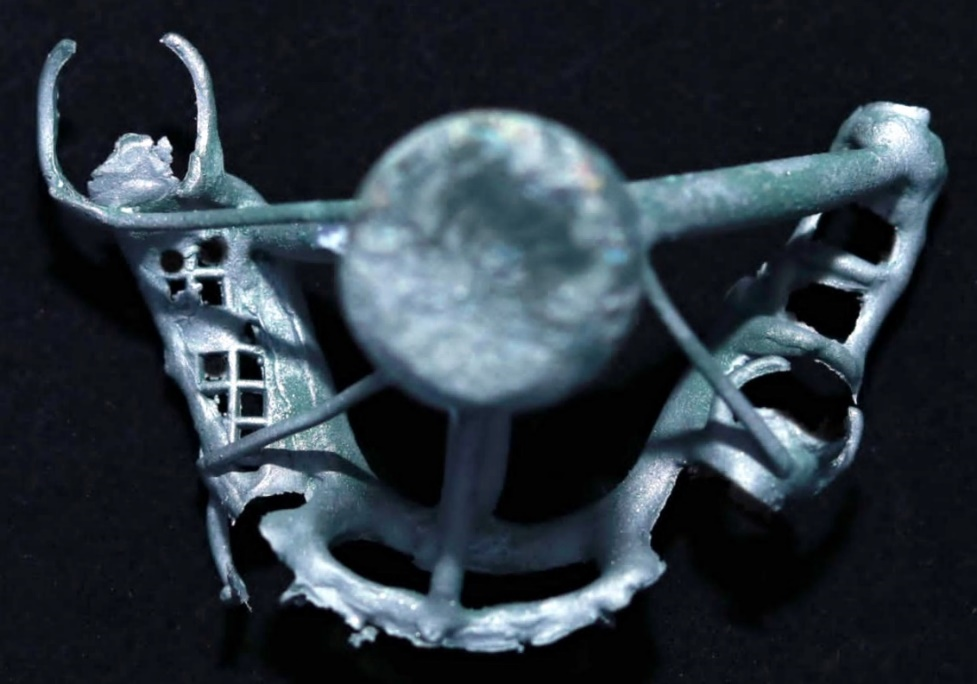
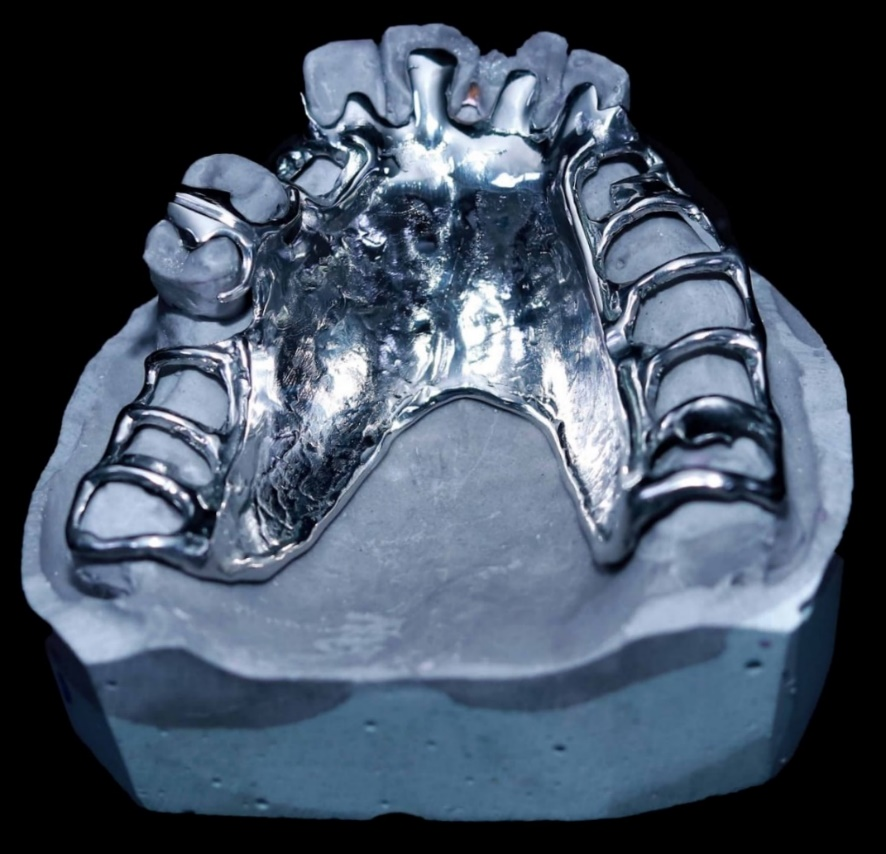
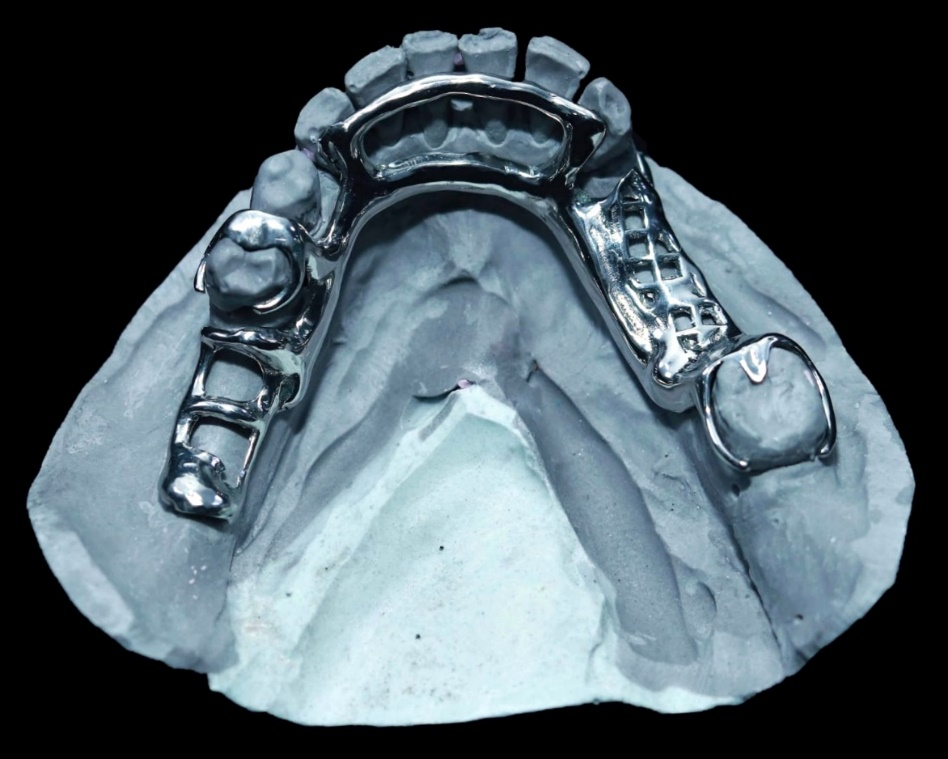
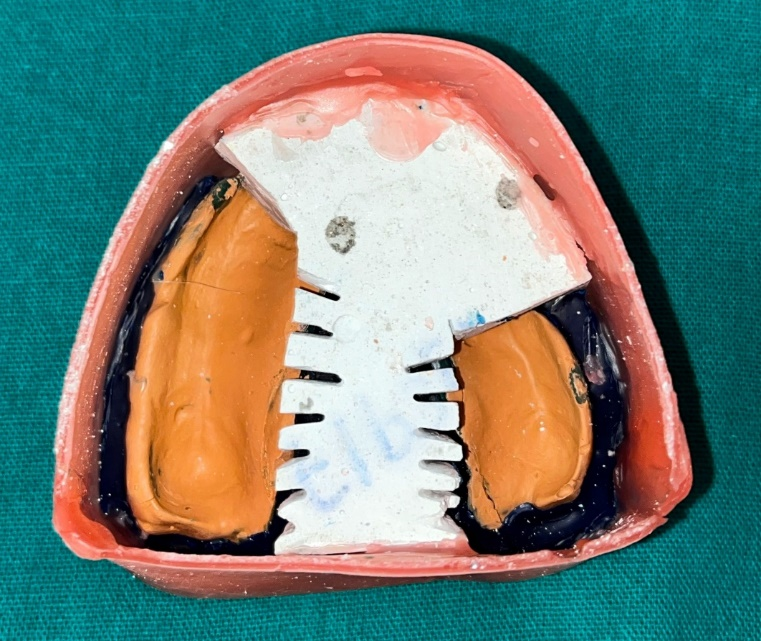
Surveying was repeated to block out unfavorable undercuts, and the master casts were duplicated to obtain refractory casts. Wax patterns (Figures 15 & 16) were created, spruing (Figures 17–20) was performed, and the framework was invested and cast (Figures 21–24). After ensuring a proper fit (Figures 25 & 26), custom trays were attached to the frameworks, and the final impression was made using zinc oxide eugenol wash impression material (DPI Impression Paste, Dental Products of India, Mumbai, India). The altered cast technique was employed, involving a saw cut distal to the remaining teeth to aid in complete seating. The cast was boxed, poured, and altered (Figures 27–37).
Figure 15. Blockout, Relief, and Wax Pattern on Maxillary Refractory Cast.
Figure 16. Blockout, Relief, and Wax Pattern on Mandibular Refractory Cast.
Figure 17. Spruing the Wax Pattern Design: Maxillary (Occlusal View).
Figure 18. Spruing the Wax Pattern Design: Maxillary (Lateral View).
Figure 19. Spruing the Wax Pattern Design: Mandibular (Back View).
Figure 20. Spruing the Wax Pattern Design: Mandibular (Lateral View).
Figure 21. Final Framework after Casting: Maxillary.
Figure 22. Final Framework after Casting: Mandibular.
Figure 23. Framework Fit on the Maxillary Cast.
Figure 24. Framework Fit on the Mandibular Cast.
Figure 25. Framework Try-In on the Maxillary Arch.
Figure 26. Framework Try-In on the Mandibular Arch.
Figure 27. Altered Cast Technique: Fabrication of Special Trays.
Figure 28. Altered Cast Technique: Maxillary Border Moulding.
Figure 29. Altered Cast Technique: Maxillary Final Impression.
Figure 30. Altered Cast Technique: Mandibular Border Moulding.
Figure 31. Altered Cast Technique: Mandibular Final Impression.
Figure 32. Altered Cast Technique: Saw Cutting of Maxillary Cast.
Figure 33. Altered Cast Technique: Saw Cutting of Mandibular Cast.
Figure 34. Altered Cast Technique: Beading of the Maxillary and Mandibular Impressions.
Figure 35. Altered Cast Technique: Boxing of the Maxillary Impression.
Figure 36. Altered Cast Technique: Boxing of the Mandibular Impression.
Figure 37. Altered Casts: Maxillary and Mandibular.
After fabricating the maxillary occlusal rim, maxillo-mandibular relations were recorded (Figure 38) and mounted. The trial denture setup was tested (Figure 39), and occlusal adjustments were made. The dentures were processed and inserted, followed by post-insertion instructions (Figures 40–45).
Figure 38. Jaw Relations.
Figure 39. Try-In Procedure.
Figure 40. Final Maxillary CPD on the Cast.
Figure 41. Final Maxillary CPD.
Figure 42. Final Mandibular CPD on the Cast.
Figure 43. Final Mandibular CPD.
Figure 44. Final Maxillary CPD in Patient’s Mouth.
Figure 45. Final Mandibular CPD in Patient’s Mouth.
Follow-up The patient was instructed on maintaining oral hygiene and was reviewed after one week for minor adjustments (Figure 46). She was subsequently reviewed at one and three months, reporting no discomfort and expressing high satisfaction with the outcome. After six months, the patient conveyed extreme satisfaction with the new cast partial dentures, appreciating their retention, stability, aesthetics, and improved mastication (Figure 47).
Figure 46. Final Maxillary and Mandibular CPD in Patient’s Mouth.
Figure 47. Post-Operative View.
DISCUSSION
Cast Partial Dentures (CPDs) have become the preferred option over conventional fixed prostheses in Kennedy Class I cases due to the absence of posterior abutments [13]. n the specific clinical case described, the patient opted for a cost-effective solution, making a conventional CPD suitable for bilateral distal extension in both the maxillary and mandibular arches. Implant-supported fixed prostheses were avoided due to their time-consuming and costly nature, insufficient bone height and width, and the patient's financial constraints [14].
Prosthodontic rehabilitation for partially edentulous patients has significantly improved with recent advancements, such as CAD/CAM technology, precision-milled attachments, implant-supported prostheses, and enhanced impression materials [15]. These innovations have greatly increased the quality and acceptance of Removable Partial Dentures (RPDs). The choice of treatment mainly depends on the condition of the abutment teeth, which are often periodontally compromised.
The Altered Cast Impression Technique is commonly utilized for maxillary as well as mandibular distal extension partially edentulous arches (Kennedy’s Class I and II) [16]. This technique addresses issues with retention and stability, as well as displacement of the mucosa under occlusal pressure. Applegate originally described the Altered Cast Technique, also known as the corrected-cast technique [17]. John B. Holmes' study on the "Influence of Impression Procedures and Occlusal Loading on Partial Denture Movement" concluded that partial denture movement due to occlusal loading is influenced by the impression technique and material used [18]. Specifically, the altered cast technique resulted in the least movement from occlusal loading at insertion, and partial dentures fabricated with the altered cast technique demonstrated the least movement overall.
The RPI Concept and I-Bar provide retention against vertical displacement, with the I-Bar's effectiveness enhanced by the parallelism of guide planes that typically restrict displacement to the path of insertion [19]. The advantages of the I-Bar include providing horizontal stability, stabilizing and reuniting the arch, and offering retention due to its parallelism, which limits dislodgement to the path of insertion. Additionally, it protects the tooth-tissue junction by preventing food impaction and providing metal coverage, while also offering good reciprocation [20].
In distal extension cases, mesial rests are placed on the mesial aspect of the abutment teeth to verticalize occlusal forces on the bearing mucosa under the denture base extension and to direct tipping forces on the abutment mesially, thereby moving the abutment tooth into firmer contact with the support of the anterior teeth. If a modification space exists, clasp the teeth adjacent to the edentulous space, using a tripod configuration [21].
Indirect retention should be maximized by placing indirect retainers as far as possible from the distal extension base to achieve better leverage. While the incisor region is the most effective location for indirect retainers, canines or premolars are often used due to the strength limitations of incisors [22]. In the mandible, retention from the denture base itself can contribute to indirect retention. Additionally, a double lingual bar resting on an unprepared lingual surface enhances indirect retention through terminal rests. Moreover, the reciprocal arm of a direct retainer positioned anterior to the fulcrum line can also function as an indirect retainer [23].
The longevity of a Removable Partial Denture (RPD) is influenced by the forces applied to the abutment teeth, which vary due to the different nature and behavior of the supporting tissues [24]. In this case, control over these forces was achieved using metal extensions from an antero-posterior palatal strap major connector, which rested on the palatal surfaces of the incisors with cingulum rests as indirect retainers, and an I-bar direct retainer on the posterior abutment teeth, complemented by a stable denture base [25]. A Cast Partial Denture (CPD) without precision attachments was selected for the rehabilitation of both the maxillary and mandibular arches due to the complex, time-consuming treatment process and the patient’s financial limitations [26].
Cobalt-chromium (Co-Cr) metal frameworks are preferred in CPD design because of their strength, good thermal conductivity, and stability, providing an optimal balance between deformation, stiffness, and elasticity [27]. Acrylic dentures with stainless steel clasps tend to deform quickly. The first Co-Cr RPD framework manufactured directly by Selective Laser Melting (SLM) for a patient was attributed to Williams et al. Digital technology, including 3D E-models, has enhanced digital designing, cast evaluation, and reproducibility, although conventional methods remain relevant with appropriate diagnosis, treatment planning, and execution [28].
For this patient, a maxillary and mandibular Cast Partial Denture (CPD) was chosen due to its excellent retention, stability, and stress distribution. Alternatives like complete dentures were avoided to prevent reduced proprioception and support, while implant-supported prostheses were not considered due to the patient’s medical condition and reluctance to undergo surgery [29]. However, limitations of removable maxillary CPDs include issues with patient adaptation, plaque accumulation around abutment teeth leading to caries and periodontal disease, and aesthetic concerns due to the visibility of metal components [30].
In Kennedy Class I cases, CPDs are preferred due to the absence of posterior abutments, which makes fixed bridgework unfeasible. Both the maxillary and mandibular CPDs were chosen for this patient based on their preference for a cost-effective and expedient treatment. Implant treatment was ruled out due to its longer duration, higher cost, insufficient bone, and the patient’s financial constraints. Stewart indicated that bilateral clasps are suitable for Class I partially edentulous arches, though they do not fully control harmful forces, which must be managed by placing indirect retainers bilaterally on canines. To minimize harmful horizontal forces on the supporting teeth and the alveolar ridge, correct fitting of the retentive and stabilizing arm of the clasp, as well as proper direction of denture insertion, are crucial. Mesial rests on the rearmost abutments increase the arch of rotation, promoting vertical forces and providing a buttressing effect [31].
Co-Cr properties offer an ideal balance between deformation, stiffness, and elasticity for long-lasting performance. Metal-based frameworks provide high strength and good thermal conductivity for a natural experience. The RPI system, which includes an I-bar retentive element, mesial rest, and distal proximal plate, minimizes torqueing forces and directs occlusal loads parallel to the long axis of abutments, reducing lateral forces. Flexible RPDs, made from nylon-based thermoplastic material, are indicated for mandibular bilateral distal extension cases with insufficient space for a lingual bar. Flexible dentures offer translucency, clear clasps for aesthetics, strength, flexibility, biocompatibility, and freedom from monomer and metal allergens found in conventional denture materials [32].
CONCLUSION
The design of distal extension removable dentures should be carefully tailored to each patient's needs, evaluating the advantages and disadvantages of various components. Restoring a partially edentulous mouth while addressing patient needs presents challenges in treatment planning. The approach used for this patient was straightforward yet provided optimal care. The maxillary and mandibular cast partial dentures offered stability, functionality, and biological restoration.
Cast partial dentures are a suitable treatment for partially edentulous patients when implant-supported prostheses and conventional fixed partial dentures are not viable. The design and selection should be based on a comprehensive clinical evaluation, considering the pros and cons of each component. Cast partial dentures effectively restore masticatory efficiency, improve aesthetics, phonetics, and function, all without complex treatment procedures. A well-maintained cast partial denture offers better retention, stability, masticatory efficiency, comfort, and periodontal health of the abutment teeth, provided that regular oral and denture hygiene is maintained. In this case, the patient’s expectations for function and aesthetics were met economically and efficiently, without resorting to invasive procedures.
REFERENCES
- Kratochvil FJ. (1963). Influence of occlusal rest position and clasp design on movement of abutment teeth. J Prosthet Dent. 13(1):114-124.
- Krol AJ. (1973). Clasp design for extension-base removable partial dentures. J Prosthet Dent. 29(4):408-415.
- Eliason CM. (1983). RPA clasp design for distal-extension removable partial dentures. J Prosthet Dent. 49(1):25-27.
- Nazarova E, Taylor TD. (2012). The RPH clasp assembly: a simple alternative to traditional designs. J Prosthodont. 21(4):331-333.
- Hakkoum MA. (2016). New clasp assembly for distal extension removable partial dentures: the reverse RPA clasp. J Prosthodont. 25(5):411-413.
- Hajjaj MS. (2019). Modified Equipoise Clasp: an esthetic option for removable dental prostheses. J Prosthodont. 28(6):724-727.
- Kukunoor S, Savadi RC, Venkata Krishnam Raju K, Kumar S. (2014). A viable treatment alternative in distal extension cases: a case report. J Indian Prosthodont Soc. 14(Suppl 1):177-180.
- Eggbeer D, Bibb R, Williams R. (2005). The computer-aided design and rapid prototyping fabrication of removable denture frameworks. J Eng Med. 219(3):195-202.
- Thakare KS, Bhongade ML, Charde P, Kale S, Jaiswal P, Somnath BK, Pendor S. (2013). Genetic mapping in Papillon-Lefèvre syndrome: a report of two cases. Case Rep Dent. 2013:404120.
- Godbole S, Phakhan AJ, Kale S, Dahane T. (2016). Prosthodontic considerations of speech in complete denture. IOSR J Dent Med Sci. 15(11):41-44.
- Mistry R, Pisulkar SK, Borle AB, Godbole S, Mandhane R. (2018). Stability in complete dentures: an overview. IOSR J Dent Med Sci. 17(11):36-41.
- Pradhan B, Joshi SP, Verma A. (2019). A viable rehabilitation approach with maxillary cast partial denture and mandibular overdenture: a case report. Journal of Nepalese Prosthodontic Society. 2(1):53-57.
- D'Souza DS, Dua P. (2011). Rehabilitation strategies for partially edentulous: prosthodontic principles and current trends. Medical Journal Armed Forces India. 67(3):296-298.
- Daniel S, Yadav R, Kumar GA. (2020). Maxillary and mandibular distal extension rehabilitation: combination of cast partial denture with RPI system and flexible partial denture: a case report. Int J Allied Med Sci Clin Res. 8(1):25-31.
- Bhathal M, Batra J, Attresh G, Sambyal S. (2015). A review on stresses induced by removable partial dentures. Int J Contemp Dent Med Rev. 2015:050115.
- Kazem NM, Abd ST, Dawood MA, Admon M, Sabah M. (2017). The effect of removable partial denture on periodontal health status. Global J Biotechnol Biochem. 6(3):512-515.
- Kuriakose EM, Aradya A, KN RS. (2019). Cast partial denture: a preferred choice of the patient over acrylic partial and flexible denture: a case report. IJARIIT. 5(3):615-617.
- Carr AB, McGivney GP, Brown DT. (2005). Removable Partial Prosthodontics. Missouri: Elsevier Mosby.
- Wagner B, Kern M. (2000). Clinical evaluation of removable partial dentures 10 years after insertion: success rates, hygienic problems, and technical failures. Clin Oral Investig. 4(2):74-80.
- Lee HE, Wu JH, Wang CH, Lan TH. (2008). Biomechanical analysis of distal extension removable partial dentures with different retainers. J Dent Sci. 3(3):133-139.
- Boçari G, Hysenaj N, Boçari A. (2014). The advantages of partial dentures made of cast framework cr-co toward those made of resin-based dentures. Int J Dent Sci Res. 2(2):32-35.
- Tawse-Smith A, Rivillas CC, Orozco PS, Diaz JE, Pack AR. (2001). Clinical effects of removable acrylic appliance design on gingival tissues: a short-term study. J Int Acad Periodontol. 3(1):22-27.
- Balwani TR, Dubey SG, Sathe S, Chandak A. (2020). Demystifying the role of phonetics in complete denture. Int J Res Pharm Sci. 11(Suppl 4):2037-2043.
- Watson CL, Reeve PE, Barnes E, Lane AE, Bates JF. (1986). The role of personality in the management of partial dentures. J Oral Rehabil. 13(1):83-91.
- Runov J, Kroone H, Stoltze K, Maeda T, El Ghamrawy E, Brill N. (1980). Host response to two different designs of minor connector. J Oral Rehabil. 7(2):147-153.
- Al-Jammali ZM, Saad Z, Saad M. (2020). Prosthodontics clinical cases (patients with decreased inter-arch distance: case report). IJMRA. 3(1):1-9.
- Crum RJ, Rooney GE Jr. (1978). Alveolar bone loss in overdentures: a 5-year study. J Prosthet Dent. 40(6):610-613.
- Rissin L, House JE, Manly RS, Kapur KK. (1978). Clinical comparison of masticatory performance and electromyographic activity of patients with complete dentures, overdentures, and natural teeth. J Prosthet Dent. 39(5):508-511.
- Grieder A, Cinotti WR. (1968). Periodontal Prosthesis. Louis, MO: Mosby.
- Phoenix RD, Cagna DR, DeFreest CF. (2003). Stewart's Clinical Removable Partial Prosthodontics. Chicago: Quintessence.
- Henderson D, McCracken WL, McGivney GP, Castleberry DJ. (1985). McCracken's Removable Partial Prosthodontics. St. Louis, MO: Mosby.
- Singh L, Kaira SL, Dayakara HR, Singh R. (2012). Flexible denture for partially edentulous arches: a case report. J Dentofacial Sci. 1(2):39-42.
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)