Previous Issues Volume 9, Issue 9 - 2024
Radiometric Analysis of Contrast Enema for Encopresis in Children: A Review Article
Michael D Levin*
Dorot. Medical Center for Rehabilitation and Geriatrics, Netanya, Israel
*Corresponding Author: Michael D Levin, Dorot. Medical Center for Rehabilitation and Geriatrics, Amnon veTamar, Netanya, Israel, Tel: 972-538281393, Email: [email protected]
Received Date: August 18, 2024
Published Date: October 28, 2024
Citation: Levin MD. (2024). Radiometric Analysis of Contrast Enema for Encopresis in Children: A Review Article. Mathews J Case Rep. 9(9):188.
Copyrights: Levin MD. (2024).
ABSTRACT
The term "encopresis," analogous to the term "enuresis," was introduced by Weisenberg in 1926 to describe those forms of fecal incontinence in which there is no organic damage to the elements involved in fecal retention. Encopresis most often occurs in children with chronic constipation. However, the pathophysiology and pathogenesis of this phenomenon are not well understood. Less commonly observed is non-retentive fecal incontinence, the etiology and pathogenesis of which are unknown. It is not accompanied by fecal retention in the rectum, and therefore, there is no constipation. Objective: To study the pathogenesis of encopresis in children using radiometric analysis of barium enemas. Material: This article is based on a review of our published studies using radiometric analysis. In 127 (77%) patients in group 1, encopresis was combined with constipation, and a barium enema revealed varying degrees of megacolon. The 39 (23%) patients in group 2 had no history of constipation and showed no dilatation of the rectum according to the barium enema. Results: In children with chronic constipation, large volumes of feces accumulate in the rectum due to delayed bowel movements. In the dilated rectum (megacolon/megarectum), large fecal masses form, stretching the pelvic floor muscles. Stretching of the puborectalis muscle (PRM) weakens fecal continence, leading to stool leakage into underwear. Various degrees of PRM dysfunction were observed, up to the development of descending perineal syndrome. In children with encopresis without constipation, a decrease in the width of the rectum and the left side of the colon was found. In most of these cases, proctoscopy revealed macroscopic signs of inflammation. We hypothesize that the inflammatory process leads to increased intestinal tone and rapid movement of the bolus into the rectum, with high rectal tone stimulating the defecation reflex with small volumes of feces. Conclusion: The data obtained on the pathogenesis of different forms of encopresis will allow for the implementation of pathogenetic treatment.
Keywords: Encopresis, Functional Constipation, Barium Enema, Nonretentive Fecal Incontinence, Pathophysiology.
INTRODUCTION
The term "encopresis," analogous to the term "enuresis," was first introduced by Weisenberg in 1926 to describe those forms of continence disorders in which there is no organic damage to the elements involved in fecal retention [1]. In childhood, the term "fecal incontinence" is most often used, which encompasses both organic damage and functional disorders [2,3]. Among modern pediatric doctors, it is well-established that: "The pathophysiology of functional fecal incontinence related to constipation in children is not clear" [4,5]. In 10% of patients, encopresis presents as a single symptom without any organic cause or sign of constipation and is currently classified as functional non-retentive fecal incontinence (FNRFI), the etiology and pathogenesis of which remain unknown [6,7]. This lack of understanding means that there is no pathogenetic treatment, and a trial-and-error approach is commonly used.
This review focuses on the radiometric analysis of children with encopresis treated at the Children's Surgical Center in Minsk (Belarus). The research materials were published between 1983 and 2020. Patients who had undergone surgery in the anorectal area, which could damage the muscles involved in fecal retention, were excluded from this study. Their fecal incontinence was considered organic in nature. All 166 patients with encopresis were divided into two groups based on the clinical picture and the results of a barium enema. In 127 (77%) patients in group 1, encopresis was combined with constipation, and a barium enema revealed varying degrees of megacolon. The 39 (23%) patients in group 2 had no history of constipation and no rectal dilatation according to the barium enema [1,8-11].
The purpose of this article is to demonstrate the effectiveness and reliability of radiometric analysis using a contrast enema in diagnosing various forms of encopresis.
METHODS
Radiometric analysis is based on a standardized barium enema technique and includes standards for the width of different parts of the colon and rectum, as well as the length of the anal canal in children of different ages (control), which were determined using this technique [12].
The study was conducted using a hydrostatic barium enema. Barium was introduced from a graduated bag, with the bottom of the bag initially positioned 40 cm above the table deck. Barium was introduced into the colon until reflux into the terminal ileum occurred. The difference in barium volume in the bag before and after colon filling corresponds to the colon's volume. A radiopaque marker was attached to the tip of the enema and remained in contact with the anus during the study. At least two radiographs (frontal and lateral) were taken after the colon was filled. On the frontal radiograph, the widths of the different parts of the colon were measured (Figure 1a). Since the rectum forms two bends in two projections, it cannot be differentiated on the frontal radiograph, making it impossible to measure its width. On the lateral radiograph, the maximum width of the vertical portion of the rectum was measured, as well as the interval without contrast medium between the rectum and the contrast marker on the posterior contour of the tip of the enema (Figure 1b). This distance is due to the contraction of the anal canal and is equal to the length of the anal canal measured during a manometric study [12].
Figure 1. (a). The frontal radiograph shows the measurement sites: c - caecum, a - ascending colon, t - transverse colon, d - descending colon, s - sigmoid colon. (b). On a lateral radiograph, the measurement location for the descending branch of the rectum is shown as (R). The length of the anal canal is measured between the rectum and a radiopaque marker located near the anus.
Filling of the colon occurs under low hydrostatic pressure, resulting in slow colonic filling that is easily tolerated by children of all ages. Therefore, in children with encopresis, there were no cases of contrast agent leakage, eliminating the need for inflating the rectal balloon. This allowed for the measurement of the anal canal's length.
Method of the analysis of the radiographs
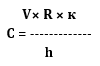
The distance between the marker (anus) and the rectum, which does not contain a contrast agent is equal to the anal canal length measured by the manometric method. This is a zone of the anal canal contraction. The true values were obtained by multiplying of the size measured on radiographs, on a factor of projection magnification (k), which is equal to the ratio of the true diameter of the marker to its value on the radiograph. To compare the different studies as well as studies of the same patient at different ages, we calculate the constant (C), which is the integral characteristic of the colon value. It is calculated using the following formula:
Where: C – constant, V – colon volume (ml).
R – rectal width (cm).
к – projection distortion factor, which is the ratio of the true width of the marker to its image on the radiograph;
h – patient height (cm).
In healthy children, "Constant" was in the range of 17-31, regardless of age. Megacolon determined if «Constant», exceeds 31. It has been possible to differentiate megacolon varying degrees depending on the constant (C):1st degree - (C = 32 - 45); 2nd degree - (C = 45-60) and 3rd degree - C> 60.
Since the sigmoid colon, after the age of 5 years, is normally located in the small pelvis, its location in the abdominal cavity always indicates elongation. The lengthening of the sigmoid colon is due to the presence of the mesentery. Since it is not fixed to the abdominal wall, it lengthens simultaneously with expansion. Thus, elongation of the sigmoid colon is evidence of overfilling of the colon with feces during megacolon or in the past, after which the volume of the intestine decreased due to the inflammatory process. The transverse colon also has a mesentery and can elongate and sag into the pelvis in very severe forms of megacolon in adults. Filling the colon prior to barium reflux into the ileum has proven to be very useful in determining the etiology and pathogenesis of functional megacolon (FM). Since the width of the rectum does not change after filling the splenic flexure, it is sufficient to fill the colon up to the splenic flexure to diagnose megarectum. Table 1 shows the normal dimensions of the rectum and anal canal, which are sufficient in practice to assess the presence of megarectum and the condition of the pelvic floor muscles, including the puborectalis muscle (PRM).
Table 1. The true rectal width and anal canal length depending on age
|
Age |
n |
Rectal width (cm) |
n |
Anal canal length (cm) |
|
5 days-11 months |
12 |
1,3-3.0 (2.24±0.09) |
7 |
1.7-2.5 (2.21±0.15) |
|
1-3 years |
9 |
3.0-3.7 (3.21±0.11) |
7 |
2.3-2.8 (2.55±0.10) |
|
4 – 7 years |
9 |
3.0-3.9 (3.43±0.14) |
8 |
2.3-3.6 (3.11±0.10) |
|
8 – 10 years |
9 |
3.2-4.1(3.70±0.06) |
8 |
2.6-3.7 (3.07±0.11) |
|
11 – 15 years |
19 |
3.6-4.6 (39.5±0.07) |
18 |
3.1-3.9 (3.43±0.10) |
It appears that the causes of chronic constipation (CC) in early childhood vary. CC very rarely begins in the first year of life, most often occurring after the cessation of breastfeeding when the stool becomes more formed. These patients rarely visit a surgical hospital in the first year of life (Figure 2A). As shown in the studies by Duhamel [13] and Clayden with Lawson [14], in some children with severe megacolon, the cause of constipation is minor anorectal malformations, such as anterior anus or anal/rectal stenosis with a relatively wide but abnormal orifice. Clayden and Lawson found secondary megacolon in 5% of children who were initially diagnosed with functional megacolon [15]. It is likely that constipation occurring in the first year of life is secondary to congenital stenosis of the anus or anal canal stenosis.
As shown in Figure 2B, functional megacolon (FM) typically begins after the first year of life during potty training, with a peak incidence between 3 and 8 years of age, during social adaptation to group settings. Encopresis typically appears 1–5 years after the onset of constipation. Figure 2C illustrates that the more severe the degree of megacolon, the more likely it is to be accompanied by encopresis [8].
Figure 2. A). Graphic representation of the frequency of megacolon depending on the time of occurrence of constipation - (a), and the time of going to the surgical hospital (b). B). Graphical representation of megacolon frequency depending on the time of onset of constipation- (a), and the time of onset of encopresis - (b). (C). The relationship between numbers of patients with encopresis - (a), and without encopresis - (b) depending on the degree of megacolon.
Analysis of the above graphs shows that encopresis primarily occurs after the age of 3, sometime after the onset of constipation, due to the progression of megacolon. The greater the degree of megacolon, the more likely it is that the condition will be complicated by encopresis. Due to the dilation of the rectum, its anterior wall is pushed forward, resulting in the absence of the lower horizontal branch of the rectum (Figure 3b-3e). This figure also shows the varying degrees of damage to the pelvic floor muscles in sequential order.
Among the patients, 83 (65%) had grade 1–2 megacolon. The length of their anal canal was within the age norm. In the initial stage of the disease, due to large fecal masses pressing against the pelvic floor muscles, swelling of the pelvic floor occurs. This is manifested by a concavity of the rectum behind the anal canal, giving the impression of its elongation [12]. In these patients, encopresis was generally not detected. Various degrees of puborectalis muscle (PRM) weakness were indicated by the presence of barium in the anorectal angle (Figure 3c). In 18 patients, barium leakage was observed in the upper part of the anal canal behind the enema tip, with the length of the anal canal near the lower limit of normal (Figure 3d). In 26 cases, a decrease in the length of the anal canal by nearly half compared to the norm was detected (Figure 3e). Encopresis in patients with functional megacolon (FM) was always accompanied by varying degrees of PRM weakness. A significant shortening of the anal canal is caused by insufficiency of the PRM and levator plates, a condition referred to in the literature as descending perineal syndrome (DPS) [16,17]. Figure 4 illustrates the mechanism of DPS development and our proposed method for diagnosing it.
Figure 3. Lateral radiographs of the anorectal area in normal conditions (a) and with FM (b-e). (a) Normally, two branches of the rectum are identified: vertical (v) and horizontal (h). The length of the anal canal is measured from the anorectal angle (arrow) to the radiopaque marker located near the anus. In the upper part of the anal canal in front of the enema tip, penetration of barium is determined, which is due to relaxation of the internal anal sphincter (IAS). The posterior wall of the anal canal at this level is pressed against the tip of the enema by the contracted PRM. The lower part of the anal canal is closed by contraction of the external anal sphincter (EAS). This is a retention reaction, which is the radiological manifestation of the rectoanal inhibitory reflex [15]. (b-c). Dilatation of the rectum is accompanied by the disappearance of the horizontal branch and the appearance of contrast material in the upper part of the anal canal behind the enema tip due to weakness of the PRM. (d-e). The expansion of the rectum is accompanied by a sharp shortening of the anal canal because of incompetent PRM.
Figure 4. A 15-year-old patient with FM and encopresis. The true diameter of the X-ray contrast marker located near the anus is 1.6 cm. The width of the fecal stone is 9 cm is 2 times greater than the maximum normal limit for the width of the rectum (4.6 cm). A peristaltic wave starting from the rectosigmoid sphincter (red arrows) pushes the stone under great pressure. However, the width of the anal canal does not allow a stone of this width to pass through. The distance between the pubococcygeal line and marker is 4 cm and it is equal to the length of the normal anal canal. However, the bougie effect of the stone led to stretching of the pelvic floor muscles (PRM and levator plates). As a result of the weakness of the PRM, only the lower part of the anal canal functions to retain feces. Therefore, liquid barium under pressure passes along the enema tip outward (shown by white lines), which manifests itself as functional fecal incontinence (encopresis).
In adults, DPS is defined as the descent of the contrast-enhanced rectum several centimeters below the pubococcygeal line during defecation. This is typically assessed through defecography [17] or MRI defecography [18-21] performed during defecation on a radiolucent potty. However, this study involves prolonged exposure to ionizing radiation and can be challenging due to the difficulty in identifying bone landmarks for drawing the pubococcygeal line. Because of these limitations, defecography is not used to diagnose DPS in children. The method described above identifies DPS as the shortening of the anal canal, measured from the marker near the anus to the barium in the intestine during a conventional barium enema.
Encopresis in children without constipation (2nd group)
Among the 39 patients in group 2 (mean age 9.2 ± 2.2 years), 37 (95%) had complaints of periodic, non-localized abdominal pain in addition to fecal incontinence. There were eight times more boys than girls in this group. In 20 (51%) patients, encopresis was combined with enuresis. During an X-ray examination using the method described above, the width of the rectum was within the age norm in only 5 (13%) cases. In the other cases, the width of the rectum and sigmoid colon was less than the minimum limit of the age norm. The descending colon was narrower than normal in 26 (67%) patients, with asymmetric haustration. These data indicated a high tone in the left half of the colon and led to the recommendation for proctoscopy. Macroscopic signs of inflammation were detected in 29 (74%) patients during proctoscopy [1].
DISCUSSION
An analysis of the literature and our research shows that patients with functional megacolon (FM) develop encopresis due to rectal overflow with feces, which is invariably accompanied by megacolon. The accumulation of large fecal masses stretches the pelvic floor muscles, leading to a weakening of their function. Without pathogenetic treatment, this process progresses from minimal damage to descending perineal syndrome (DPS), which ultimately causes encopresis. DPS represents irreversible damage that can only be treated with puborectalis muscle (PRM) plication or gracilis muscle transposition. Symptomatic treatments, such as bowel management, including antegrade enemas for DPS, complicate patients' lives. Additionally, the stretching of the levator plates disrupts the function of opening the anal canal during defecation attempts, significantly increasing resistance to fecal movement through the anal canal. This is one of the contributing factors to the chronicity of FM.
The differentiation between encopresis in FM and nonretentive encopresis has been based solely on the absence of a history of constipation. No diagnostic method has proven to be fully accurate. Since the etiology of this condition was unclear, treatment approaches cannot be considered pathogenetic, especially since none of the currently used methods have shown significant breakthroughs. For example, guidelines approved with a “high consensus” include only one statement: “Laxatives can worsen outcomes and should be avoided” [22]. When using biofeedback and/or laxative treatment, only 29% of patients were successfully treated after two years of intensive therapy. Despite improvement in most patients beyond puberty, 15% continued to experience fecal incontinence at age 18 [23]. It has also been found that temporarily adding additional rectal enemas does not significantly improve treatment success compared to conventional therapy alone, which consists of education, a non-accusatory approach, and a toileting program that includes a daily bowel diary and a reward system [24]. Special attention is recommended for psychosocial or behavioral problems, as these frequently occur in affected children [25]. However, Jørgensen et al. found that transanal irrigation was effective in a small number of children with encopresis [26]. Positive effects have also been observed with the use of transcutaneous functional electrical stimulation [27-29] and transcutaneous posterior tibial nerve stimulation [7]. Trial-and-error treatment results in “significant (p < 0.05)” symptom relief in some patients, according to their questionnaire responses. However, symptoms often do not disappear completely, and in some cases, they reappear after some time. It is known that laxatives can exacerbate symptoms.
Our data indicate that encopresis without constipation is clinically characterized by periodic, non-localized abdominal pain, an urgent need to defecate with an inability to prevent defecation, frequent co-occurrence with enuresis, and a significant predominance in boys. X-ray analysis revealed that in 13% of patients, the rectal width was within normal limits, while in 87%, the rectal width and the left side of the colon were below the minimum age norm, indicating high tone in these areas. In 74% of cases, macroscopic signs of inflammation were observed in the rectum and/or sigmoid colon. The combination of clinical and radiological symptoms provides insight into the pathophysiological process. Inflammation leads to an increase in the tone of the left side of the colon and rectum, causing the fecal bolus to move rapidly into the rectum. Since the threshold for defecation pressure in a narrow rectum is reached at a smaller bolus volume, a rapidly introduced bolus triggers a defecation reflex as quickly as in acute diarrhea. This understanding of the pathophysiology of encopresis without constipation explains why laxatives, which further increase the already high intestinal tone, exacerbate the symptoms of encopresis. In this context, loperamide has a beneficial effect by slowing intestinal motility and increasing anal canal tone. Based on the data presented, there is reason to believe that anti-inflammatory treatment, either orally or through transanal irrigation, may be effective in children with encopresis without constipation.
CONCLUSION
Encopresis in children, defined as fecal incontinence of a functional nature, can be divided into two distinct conditions with different origins. In most cases, it occurs in children with chronic constipation, where delayed defecation leads to the accumulation of large fecal masses in the rectum. In the dilated rectum (megacolon or megarectum), fecal stones form, which stretch the pelvic floor muscles. Stretching of the puborectalis muscle (PRM) weakens fecal continence, leading to the leakage of feces into underwear. Varying degrees of PRM dysfunction have been observed, ranging from minimal impairment to the development of descending perineal syndrome. In children without constipation, a reduction in the width of the rectum and left side of the colon has been found. In most of these cases, proctoscopy revealed macroscopic signs of inflammation. High intestinal tone causes rapid advancement of the fecal bolus into the rectum, and the increased rectal tone triggers the defecation reflex with even small volumes of feces. This creates a situation like acute diarrhea, where bowel movements occur quickly and uncontrollably. These two forms of encopresis can be differentiated using radiometric analysis of barium enema, allowing the use of pathogenetic treatment.
REFERENCES
- Levin MD. (1986). Rentgenologicheskoe issledovanie tolstoĭ kishki i anorektal'noĭ zony pri nederzhanii kala u deteĭ [Roentgenologic examination of the large intestine and anorectal area in children with fecal incontinence]. Pediatriia. (5):35-38.
- Levitt MA, Peña A. (2010). Pediatric fecal incontinence: a surgeon's perspective. Pediatr Rev. 31(3):91-101.
- Baaleman DF, Vriesman MH, Lu PL, Benninga MA, Levitt MA, Wood RJ, et al. (2023). Long-Term Outcomes of Antegrade Continence Enemas to Treat Constipation and Fecal Incontinence in Children. J Pediatr Gastroenterol Nutr. 77(2):191-197.
- Rajindrajith S, Devanarayana NM, Benninga MA. (2013). Review article: faecal incontinence in children: epidemiology, pathophysiology, clinical evaluation and management. Aliment Pharmacol Ther. 37(1):37-48.
- Nurko S, Scott SM. (2011). Coexistence of constipation and incontinence in children and adults. Best Pract Res Clin Gastroenterol. 25(1):29-41.
- Burgers R, Reitsma JB, Bongers ME, de Lorijn F, Benninga MA. (2013). Functional nonretentive fecal incontinence: do enemas help? J Pediatr. 162(5):1023-1027.
- Abdelrahman EM, Mohamed AG, Abdel Ghafar MA, Ahmed ME, Ali RR, Kharoub MS. (2024). Long-Term Outcome of Transcutaneous Posterior Tibial Nerve Stimulation in the Treatment of Functional Non-Retentive Fecal Incontinence in Children. Surg Innov. 31(1):33-41.
- Levin MD, Misharev OS. (1983). Funktsional'nyĭ megakolon u deteĭ [Functional megacolon in children]. Pediatriia. (8):20-24.
- Levin MD. (1989). Funktsiona'lnyĭ megakolon u deteĭ [Functional megacolon in children]. Pediatriia. (8):22-27.
- Levin MD. (2015). [Descending perineum syndrome in children: Pathophysiology and diagnosis]. Vestn Rentgenol Radiol. 5:27-35.
- Levin MD. (2018). Pathophysiology and diagnosis of descending perineum syndrome in children. Pelviperineology. 37(2):52-56.
- Levin MD. (2019). Radiological anatomy of the colon and rectum in children. Gastroenterology & Hepatology. 10(2):82-86.
- Duhamel B. (1969). Physio-pathology of the internal anal sphincter. Arch Dis Child. 44(235):377-381.
- Clayden GS, Lawson JO. (1976). Investigation and management of long-standing chronic constipation in childhood. Arch Dis Child. 51(12):918-923.
- Levin MD. (2021). Anatomy and physiology of anorectum: the hypothesis of fecal retention, and defecation. Pelviperineology. 40(1):50-57.
- Wang XJ, Chedid V, Vijayvargiya P, Camilleri M. (2020). Clinical Features and Associations of Descending Perineum Syndrome in 300 Adults with Constipation in Gastroenterology Referral Practice. Dig Dis Sci. 65(12):3688-3695.
- Payne I, Grimm LM Jr. (2017). Functional Disorders of Constipation: Paradoxical Puborectalis Contraction and Increased Perineal Descent. Clin Colon Rectal Surg. 30(1):22-29.
- Lalwani N, Moshiri M, Lee JH, Bhargava P, Dighe MK. (2013). Magnetic resonance imaging of pelvic floor dysfunction. Radiol Clin North Am. 51(6):1127-1139.
- Guo M, Zbar AP, Wu Y. (2023). Imaging the levator ani and the puborectalis muscle: implications in understanding regional anatomy, physiology and pathology. Scand J Gastroenterol. 58(11):1295-1308.
- Levin MD. Functional megacolon in children. Available at: https://www.anorectalmalformations.com/_files/ugd/4d1c1d_a41e68ac8aab479d9bb38ef9e5c77ced.pdf
- Guo M, Zbar AP, Wu Y. (2023). Imaging the levator ani and the puborectalis muscle: implications in understanding regional anatomy, physiology and pathology. Scand J Gastroenterol. 58(11):1295-1308.
- von Gontard A, Claßen M. (2023). Functional Constipation and Nonretentive Fecal Incontinence in Children and Adolescents: Clinical Guideline for Assessment and Treatment. Z Kinder Jugendpsychiatr Psychother. 51(3):233-250.
- Voskuijl WP, Reitsma JB, van Ginkel R, Büller HA, Taminiau JA, Benninga MA. (2006). Longitudinal follow-up of children with functional nonretentive fecal incontinence. Clin Gastroenterol Hepatol. 4(1):67-72.
- Burgers R, Reitsma JB, Bongers ME, de Lorijn F, Benninga MA. (2013). Functional nonretentive fecal incontinence: do enemas help? J Pediatr. 162(5):1023-1027.
- Koppen IJ, von Gontard A, Chase J, Cooper CS, Rittig CS, Bauer SB, et al. (2016). Management of functional nonretentive fecal incontinence in children: Recommendations from the International Children's Continence Society. J Pediatr Urol. 12(1):56-64.
- Jørgensen CS, Kamperis K, Modin L, Rittig CS, Rittig S. (2017). Transanal irrigation is effective in functional fecal incontinence. Eur J Pediatr. 176(6):731-736.
- Ladi-Seyedian SS, Sharifi-Rad L, Alimadadi H, Nabavizadeh B, Manouchehri N, Allahverdi B, et al. (2022). Comparative Efficacy of Transcutaneous Functional Electrical Stimulation With or Without Biofeedback Therapy on Functional Non-retentive Fecal Incontinence in Children: A Randomized Clinical Trial. Dig Dis Sci. 67(3):989-996.
- Read M, Read NW, Duthie HL. (1980). In: Gastrointestinal Motility. New York. pp.503-504.
- Voskuijl WP, van Ginkel R, Taminiau JA, Boeckxstaens GE, Benninga MA. (2003). Loperamide suppositories in an adolescent with childhood-onset functional non-retentive fecal soiling. J Pediatr Gastroenterol Nutr. 37(2):198-200.
.png)
.png)
.png)
.png)