Previous Issues Volume 8, Issue 4 - 2023
Pattern of Psychiatry Referrals in a Tertiary Hospital Teaching Set-up
Sumeesha Jaswal1,*, Harsh Garg2, Apanpreet Kaur2
1Senior Resident, Department of Psychiatry, Indira Gandhi Medical College and Hospital, Shimla, Himachal Pradesh, India
2Junior Resident, Department of Psychiatry, Indira Gandhi Medical College and Hospital, Shimla, Himachal Pradesh, India
*Corresponding Author: Sumeesha Jaswal, Senior Resident, Department of Psychiatry, Indira Gandhi Medical College and Hospital, Shimla, Himachal Pradesh, India; Email: [email protected]
Received Date: November 3, 2023
Publication Date: December 1, 2023
Citation: Jaswal S, et al. (2023). Pattern of Psychiatry Referrals in a Tertiary Hospital Teaching Set-up. Mathews J Psychiatry Ment Health. 8(4):45.
Copyright: Jaswal S, et al. © (2023)
ABSTRACT
Background: High rates of psychiatric morbidity to the tune of 20-65% are seen in medico-surgically ill patients but there is lack of research on concordance rates between Psychiatrist and Non- psychiatrist diagnoses of patients seen under Consultation liaison patients, especially in general hospital settings. Aim: To analyse pattern, reason of referrals, diagnostic and management concordance in patients with psychiatric morbidity in medico-surgical setting. Material and Methods: 2476 consecutive referrals received during a period of 6 months (1.11.2022-31.04.2023) in consultation liaison (CL) services in department of Psychiatry at a general hospital teaching institute were evaluated for reason of referral, psychiatric diagnosis and management given by the referring team vis-à-vis the CL team. Results: Emergency and inpatient referral rate was 0.77 % and 0.23%. Medicine and allied departments utilized CLP services majorly (51.3%), 1/4th referrals were for psychiatric emergencies (24.7%). 41.1% of referrals were requested even before primary treating team zeroed on the body organ system involved followed by multisystem involvement in 18.96% referrals. Most common diagnosis made by CLP team was substance use disorder (25.44%), anxiety disorder (20.39%), depression (12.27%), delirium (9.3%) and 4.4% being nil psychiatry. Diagnostic concordance for major psychiatric diagnoses between medicine/ surgery team and CLP team was fair in substance use disorder and anxiety disorders. Conclusion: The study findings suggest that substance use disorder is the most common diagnosis made by CLP team with a fair diagnostic concordance between medicine/surgery team and CLP team for substance use disorder and anxiety disorders. Oral/ parenteral psychotropic drugs were given in one third of cases even before CLP referral was initiated, resulting in higher frequency of side effects.
INTRODUCTION
World Mental Health Survey has reaffirmed that common mental disorders are a significant contributor to global mental health burden, with prevalence estimates of 18.1-36.1% for anxiety, mood and substance use disorders [1]. Yet, worldwide, they remain inadequately diagnosed and treated, with only a small percentage presenting to mental health specialist settings. Mental disorders are nearly twice as common (41.3% to 46.5%) in the context of physical disorders with high rates of psychiatric morbidity to the tune of 20-65% seen in medico-surgically ill patients, especially in general hospital settings compared to community or primary health care settings (CTP) suggesting the need for greater linkages between care for mental and physical disorders [2]. Consultation-liaison psychiatry (CLP) is one subspecialty of psychiatry which deals with clinical, teaching and research activities of psychiatrists, allied mental health professionals and medico-surgical professionals in the non-psychiatric divisions of a general hospital. The Consultation model largely followed in India deals with evaluation and needful management of patients in non-psychiatric units by psychiatrists on referral requests made by the medico-surgical teams [3,4]. Methodological differences exist in literature in the form of variable study duration (ranging from 1 month to more than a year), sample size, setting (only inpatients or only emergency setting or both), description of psychiatric morbidity in patients with medico-surgical illnesses or psychiatric morbidity in one specific speciality (e.g. depression in patients with cardiac illness or stroke) and very few studies have evaluated reasons of referral, diagnostic concordance for psychiatric morbidity in medico-surgical settings [4]. Common diagnoses in CLP set up in western countries are mood disorders, stress‑related disorders, whereas in Indian population, organic mental disorder is more common [5–9]. Approximately 30% of all patients in general medical settings exhibit psychiatric disorders, delirium in 10% of medical inpatients and 30% in certain high-risk patients. An alarming two-thirds of high-frequency users of medical services have a psychiatric disorder, most commonly depression (23%), anxiety (22%), and somatization disorder (20%) [7]. Indian studies have reported that in approximately half of all referrals, the medico-surgical teams had already made a diagnosis, with depression, substance abuse and delirium being among the commoner ones. Another study found that delirium followed by depression were the most common diagnosis made by the CLP team [4]. CLP referral rates of around 0.06%-3.6 % are reported for medico-surgical inpatients whereas, it is 1.42%-5.4% in emergency settings.6 Despite high psychiatric morbidity in medico-surgically ill patients both as inpatients and/or emergency settings, it largely remains underrecognized/ misdiagnosed and undertreated leading to burden of care and poorer outcomes for the patients.
In this background, the current study aimed to identify pattern of psychiatric morbidity, reasons of referral and diagnostic and management concordance between medico-surgical team and CLP team. This data shall be instrumental as a measure of psychiatry training during under-graduation and shall be helpful in gaining insight into the various shortcomings in the pattern of referrals in a tertiary care teaching hospital of North India, thereby paving way for improvement.
METHODOLOGY
Setting
The study was carried out in the Department of Psychiatry of a tertiary government medical college & hospital in North India which provides 24 hours CLP services for emergency and inpatients of non-psychiatric units of the hospital. Any patient referred to CLP services are evaluated by a junior resident (MD Psychiatry trainee) under supervision of a senior resident (MD Psychiatry) before finalizing the diagnosis and formulating a treatment plan. The referring team is requested to mention the reason(s) for referral, tentative medico-surgical diagnosis, tentative psychiatric diagnosis (if they have considered one) and treatment initiated (both for medico-surgical illness and psychiatric symptoms) while sending the referral request. Socio-demographic and clinical details are recorded in a specifically designed semi structured referral proforma including socio-demographic details, brief history of medical and present psychiatric illness, personal history, substance history, MSE, general physical examination, details of investigations, provisional diagnosis, plan of management and follow up notes for each patient seen in CLP services. Further, an online register is maintained to record all referral requests received and the details thereof.
PROCEDURE
A retrospective chart review was done for all referral requests received by CLP services from non-psychiatric units (emergency and medico-surgical inpatients) of the medical college & hospital between 01nd November, 2022 to 31st April, 2023 (6 months). The details of the referral requests were gathered from referral proforma and referral register maintained as a part of CLP services. The study was approved by institutional ethics committee.
Analysis
Data was analysed using Statistical Package for Social Scientists version 22 (SPSS version 22, SPSS Inc., Chicago, IL, USA). Descriptive data was analysed using frequency, percentage, mean and standard deviation and Cohen kappa coefficient statistics was applied to determine the diagnostic concordance between the diagnoses made by CLP team and any psychiatric diagnosis considered by medico-surgical team.
RESULTS
A total of 268,872 patients were registered in the hospital emergency services, during the study period and 116719 patients were admitted in all the departments. CLP services were requested for a total of 2697 patients, of which 221 had to be excluded (due to lack of information by the referring medico-surgical specialists), thus N=2476 patients made the final study sample. Emergency referral rate, that is patients referred from various emergencies to CL Psychiatry was 0.83% (N=2078), ward referral rate was 0.23% (N=619). The rate was calculated from the total referral calls received whereas, other analyses were computed for 2476 patients. Latency period i.e., the time taken for referring patients from various emergencies was on an average 1.75 days and from wards it was 8.3 days, which could be a reflection of a correlation between symptom severity (both medical and surgical) and need for referral.
Three fifth of the study subjects were males (N=1510; 60.9%) with a mean age of 31.2 years (SD: 29.45; range: 8-83years). 63% were married and majority resided within a 50 km radius from the medical college & hospital.
Figure 1: Pattern of utilization of CLP services by various departments.
Figure 1 highlights that more than half of the calls were from medicine and allied department (n=1272; 51.3%) followed by one fourth calls made for patients with known psychiatric illness (n=613; 24.7%) for worsening of either the psychiatric symptoms or for medico-surgical complaints. Other departments constituted a minority in utilizing CLP services, namely surgery (n=257;10.3%), Intensive care unit (n=173;6%), obstetrics & gynaecology (n=114; 4%).
Figure 2: Body organ system break up of cases referred to CLP services.
Figure 2 highlights that in 41.1 % (n=1018) of referral calls made to CLP services, the treating team maximum had still not zeroed on the organ system involved. Another 19% (n=468) had multisystem involvement followed trauma and neurological involvement in 7.87% (n=195) & 7.83% (n=194). Utilization of CLP services was lesser from the departments of pulmonary medicine (5.65%; n=140), gastroenterology (4.06%; n=100), cardiology (3.67%;n=91), operation theatre setting (3.08%;n=76) and renal system (1.97%; n=49).
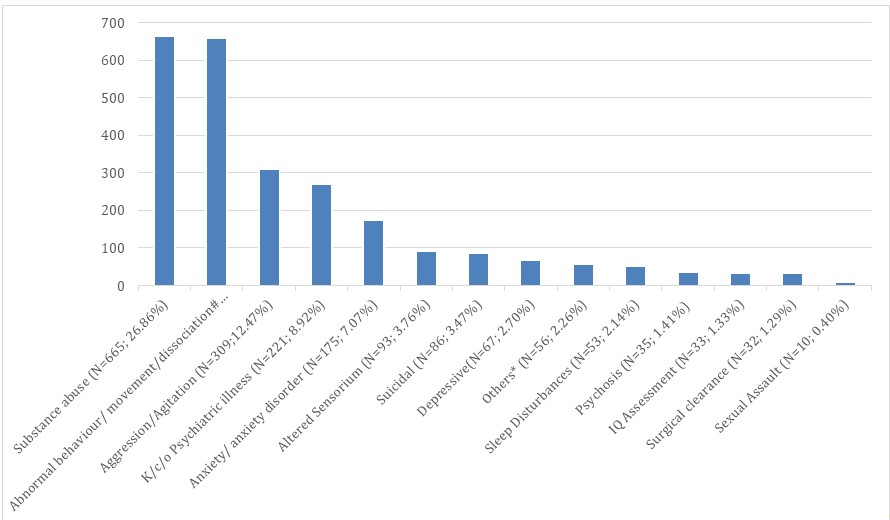
As shown in figure 3, in all cases either a specific diagnosis or specific symptom was mentioned as the reason for referral. In about one fourth of the cases each, substance abuse (n=665; 26.86%) & abnormal behaviour/movement/dissociation (n=658;26.58%) was cited. Aggression was mentioned in around 12.5% (n=309) of cases. Around 11% (n=271) of calls were made for patients known to suffering from psychiatric illness, 7% mentioned anxiety/ anxiety disorder, 3.76% (n=93) altered sensorium, 3.47% (n=86) suicidal as the reason for referral calls. Reason for call such as not accepting meals, refusing for investigations, wanting discharge constituted 2.26% (n=56), sleep disturbance (2.14%; n=53), psychosis (1.41%; n=35), sexual assault (0.40%; n=10). Psychiatric clearance for surgical procedure was mentioned for 1.29% (n=32) and IQ assessment in 1.33% (33) of cases.
Figure 3: Reasons for referral as reported by the referring medico-surgical team.
#included cases with episodes of unresponsiveness, abnormal movement, loss of function of a body part, functional emesis.
*included cases refusing meals for unknown reasons, non-cooperative e.g. asking for discharge, refusing investigations/interventions, exaggerated response to stimulus.
Most common diagnosis made by the CLP team was substance use disorder (n=630; 25.44%) followed by anxiety disorders (n=505; 20.39%), affective disorders mainly comprising depressive disorders [current episode] (n=304;14.70%) and psychotic disorders (n=297;11.99%). Delirium was made in 9.36% (n=232) of cases. 4.4% of cases for whom CLP services were sought had no psychiatric disorder. Other details are given in Figure 4.
Figure 4: ICD 10 diagnosis made by CLP team.
Diagnostic concordance between CLP team and medico-surgical team
The CLP team made a diagnosis of substance use disorder in 630 cases compared to 665 cases made by referring team. Diagnosis of delirium was considered in 93 cases by the referring team whereas, the CLP team made the diagnosis of delirium in 176 cases. Diagnosis of depression was made by CLP team in 304 cases whereas 67 referrals were sought for the same. In case of anxiety disorders 175 referrals were received and 179 were diagnosed with anxiety spectrum disorders, similarly for DSH/ Suicidal behaviour 86 referrals were received, whereas, 109 patients were diagnosed with the same. The findings are highlighted in table 2.
Table 1: Concordance rate for psychiatric diagnosis between referring Physician and Psychiatrist.
|
Diagnosis |
N (psychiatrist diagnosis) |
N’ (medico-surgical specialist diagnosis) |
Non-Concordance rates |
|
SUD |
630 |
665 |
+ 5.55 % |
|
Delirium/organicity (F05; Post-ictal/stroke confusion, etc) |
176 |
93 |
- 30.68 % |
|
Depression |
304 |
67 |
-77.96 % |
|
Anxiety spectrum |
179 |
175 |
- 2.23 % |
|
Suicidal/DSH |
109 |
86 |
- 12.84 % |
|
Psychotic spectrum |
297 |
35 |
- 88.21 % |
The negative sign implies the under identification and positive implies over identification by the referring department. The Non-concordance rates have been calculated as percentage of the difference of subtracting the two variables, divided by the value of diagnosis made by Psychiatrist.
Management by referring medico-surgical team before CLP referral
254 cases had already received injection haloperidol 5 mg before CLP services were requested for. Out of them, 22% (n=55) developed side effects (extrapyramidal symptoms), most commonly dystonia. The only reason cited for administering injection haloperidol was to control aggressive behaviour. Injection promethazine 50 mg was given to 27 cases, injection diazepam 10 mg to 43 cases, injection lorazepam 4 mg to 36 patients before CLP referral was initiated. However, none of the drugs were given in combination parenterally. Chlordiazepoxide 25 mg/day along with oral Thiamine 100mg/day was prescribed to majority of 346 patients who had presented with alcohol withdrawal, irrespective of the severity of alcohol withdrawal. Much higher doses than required of tramadol was prescribed (both oral & parenteral) for opioid withdrawal.
Table 2: Treatment initiated by medico-surgical team before CLP referral
|
Treatment initiated |
Number |
Reason(s) |
Route |
Outcome |
|
Haloperidol |
254 |
Aggression |
Parenteral |
EPS (55) Dystonia (28) |
|
Benzodiazepines |
346 |
Aggression, Alcohol Withdrawal, Anxiety, Insomnia |
Oral (N=124) (chlordiazepoxide > Clonazepam) Parenteral (N= 222) (diazepam > Lorazepam) |
Inadequate sedation (26) Inadequate alcohol withdrawal control (50) Sub therapeutic dose (25) or High dose (42) Developed Delirium (13) |
Management by the CLP team
Benzodiazepines were the most commonly prescribed drug by the CLP team in 42% (n=1762) cases followed by treatment for substance use disorder in 14.1 % (n=588). Antipsychotic medication was prescribed to 13% (n=542) cases and antidepressants/ antianxiety drugs to 11.2% (n=469) cases. Use of injectables by CLP team was limited to 4.4% (n=186) cases only. 3.2% (n=134) cases were attached to psychiatry outpatient department for non- pharmacological management.
DISCUSSION
The present study suggests that the referral rates ranged from 0.23%-1.08% stratified categorically. According to national data, the referral rate ranges from 0.06% to 5.4 %, in studies over the past 60-70 years , with 0.01%-3.6% referrals form inpatient settings and slightly higher figures (1.42%- 5.4%) for referrals form emergency settings [6]. Western literature reports inpatient referral rate of 12.1 %10 to 4.2 % [8]. The findings of the current study are comparable to the findings of most of the earlier national studies, however differences with respect to western literature can be due to different models of care followed in CLP in western countries [8,10].
The findings of the index study reflect that majority utilization of CLP services was from medicine & allied departments. It also reflects the extent of high psychiatric morbidity in medically ill population as reported in other studies [6,11] and better recognition of psychiatric morbidity by medical specialists as compared to surgical and allied specialties. It emphasizes the need of a regular consultation liaison service with medicine and allied specialities. The findings also highlight that patients already on treatment for psychiatric disorders also visit the general emergency which reflects the need of round the clock psychiatric emergency services alongside general emergency services and in addition to consultation liaison services. Other referring disciplines were surgery & allied specialities, intensive care unit, paediatrics, obstetrics- gynaecology. Although various studies on pattern of psychiatric referral have analysed referring departments, but very less focus has been given to the primary organ system involved. Our study shows that in 41% of cases the underlying pathology was still not ascertained prior to sending referral request to CLP services. This reflects that probably these were patients for whom CLP services were sought at emergency where referring clinician tend to follow a dichotomous approach i.e. organic versus functional and their preference for excluding psychiatric disorders first in order to make a clinical diagnosis. It also reflects the poor knowledge and understanding of referring physician about biopsychosocial model of psychiatric illness. Another close to 20% have multiorgan system involvement highlighting the need for prompt multidisciplinary evaluation including close liaising amongst different departments, including psychiatry to curtail loss of time to come to a provisional diagnosis and needful management. The only study reporting this shows multiorgan involvement (21.5%) was the most common cause for seeking CLP [4].
The most common reason for seeking CLP services was for deaddiction (substance use disorder) in one fourth of cases followed by abnormal behaviour/movements/dissociation as a combined category, anxiety disorders, depression and organic mental disorder. The findings are consistent with earlier study conducted in the same set up [5,12]. but slightly different from studies across the country, in which the most common reasons were neurotic symptoms, organic mental disorders or depression [4,13–15]. A plausible explanation for differing findings could be that the exact reason as mentioned by referring team was noted which could be more impressionistic rather than the actual reason e.g. abnormal behaviour reported by the referring team could be a presentation of dissociative disorders as well as organic mental disorders. Similar findings to the index study with respect to self-harm are reported in other Indian studies [13,16,17]. Another Indian study inferred that comorbid psychiatric illness was the commonest reason for referral (32.6%), followed by intentional self-harm (30.3%) and medically unexplained symptoms (19.3%).13 These findings do not resonate with the index study and may be explained on the basis of difference of methodology, setting and sample size (135 v/s 2476) and also the fact that the institute where the study was conducted is a multi-speciality teaching hospital catering to many referred patients from the neighbouring states. The difference in the figures of self-harm in the index study could be attributed to due to inclusion of patients both from emergency as well as inpatients units compared to other studies in which only inpatients were included. It may be hypothesized that either facts regarding the acts of self- harm were concealed or CLP services were not called for due to high lethality rates of most commonly used methods of suicide in North India (i.e hanging and organophosphate poisoning). The lower rates of Delirium in our study could be associated with early identification and prevention of subsequent delirium, or higher rates of hypoactive delirium, therefore lower reporting of any problematic behaviours by physicians as well as family members and thus not availing CLP services.
Substance use disorder was the most common psychiatric diagnosis made by the CLP team. The NMHS survey also reported higher prevalence of SUD in northern India to the tune of 1-40%.18 Anxiety disorders constituted the next common diagnosis made by CLP team followed by affective and psychotic disorders. Most of the Indian studies, especially from North India have reported substance use disorder as the most common psychiatric diagnosis followed by depression and intentional self-harm [6,13,19–21] To summarise SUD, anxiety and depressive disorders, psychotic disorders and organic brain syndrome were amongst the top five diagnoses, with our study finding high rates of psychotic disorders also amongst the common diagnoses. Western literature reports anxiety disorder and depression as common diagnoses in referral services [9,22]. A European study including 11 countries depicted self-harm as the most common diagnosis, and a German study depicted organic mental disorders as the most common diagnosis [8,9,19,22]. Various plausible explanations of a difference in findings of the index study with previously conducted national and international studies could be due to patients with depressive disorders seeking direct help from psychiatry outpatient services, increased knowledge and comfort of medico-surgical specialists in prescribing anti-depressants or conversely, ignorance/under-training of residents in non-psychiatric units regarding early identification of symptoms which could be due to other causes e.g. hypoactive delirium mimicking depression. Also ethnic variations could play a role.
Despite the availability of 24*7 CLP services, a substantial number of patients had received parenteral haloperidol for aggression/agitation before initiation of referral. 22% of these cases developed EPS, highlighting adverse events reflecting lack of knowledge of psychotropic use. Even before initiating referral, the patients were prescribed Tablet Thiamine and/or a benzodiazepine for alcohol withdrawal, most commonly chlordiazepoxide but at lower dose than required for combating withdrawal and without taking into account time of last intake and/or daily units of consumption. 35% patients of opioid use disorder were started on i/v Tramadol infusion, before CLP referral, complicating the detoxification/substitution therapy, leading to adverse events and prolonged hospital stay. A previous study assessing the usage of psychotropics by non-psychiatrists reported a rate of 10.73%. Non-psychiatrists [55.3%] commonly prescribed psychotropics of which benzodiazepines [27.43%] were the preferred drugs, whereas psychiatrists prescribed different class of psychotropic drugs [21]. The psychotropic preference of usage by the medicine/surgery team in the index study was antipsychotics followed by benzodiazepines. The commonly prescribed drugs depend on the Government supply of free psychotropics and availability and preference of the physician based on knowledge and experience. Such findings add extra cost of hospital stay and undue side effects in patients and further time required for slow taper of various psychotropics, to stabilise the patient and start treatment after comprehensive psychiatric evaluation.
Diagnostic concordance between medicine/surgery team and CLP team was “fair” for SUD and anxiety disorders in the index study and “poor” for diagnoses of delirium, psychotic disorders where the CLP team diagnosed substantially more number of such disorders in the referred cases. Concordance rates for SUD are reported to be moderate in literature. The findings are consistent with other studies reporting low ICD 10 diagnostic concordance between referring team and the CLP team which indirectly reflects poor knowledge, underdiagnosis/misdiagnosis at the hands of referring team [23].
The diagnostic concordance for delirium was dismally low in the current study which is in line with other studies focussing on delirium [15,22,24]. These findings attract extra concern because of high morbidity and mortality in delirium.
The findings of the index study highlight high psychiatric comorbidity in non-psychiatric units of a hospital [2]. Medico-surgical specialists usually focus on illness suggested by physical examination and investigations, often missing psychiatric morbidity. Lack of knowledge and interest, poor attitude in non-psychiatric specialists contribute to the current findings highlighting need and responsibility of CLP team in improving the knowledge and attitude of medical/surgical specialist towards psychiatry.
Though the study has strengths of large sample size of referrals patients from indoor and emergency set up of tertiary care teaching hospital and analysed the concordance rate of diagnoses between non-psychiatrist and psychiatrist but has certain limitations of retrospective in nature and Cohen’s kappa statistics could not be applied due to methodological limitations.
CONCLUSION
The index study reported the referral rate for psychiatric consultation from 0.25-1.08 % at non- tertiary care teaching hospital setting. Department of medicine was the major referral department. The concordance rates for diagnosis of substance use disorder and anxiety disorders were ‘fair’ whereas it was ‘poor’ for diagnoses of delirium, psychotic disorders between referring doctor and CLP team. Inadvertent and inadequate doses of psychotropic use by non-psychiatrist led to sides effects and under control of substance withdrawal.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- Kessler RC, et al. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiol Psychiat Sci. 18:23–33.
- Rothenhäusler HB. (2006). Mental disorders in general hospital patients. Psychiatr Danub. 18:183–192.
- Lipowski ZJ. (1983). Current trends in consultation-liaison psychiatry. Can J Psychiatry Rev Can Psychiatr. 28:329–338.
- Grover S, Sahoo S, Aggarwal S, Dhiman S, Chakrabarti S, Avasthi A. (2017). Reasons for referral and diagnostic concordance between physicians/ surgeons and the consultation-liaison psychiatry team: An exploratory study from a tertiary care hospital in India. Indian J. Psychiatry 59:170.
- Sidana A, Sharma R, Chavan B, Arun P, Raj L. (2009). Psychiatric profile of patients attending General Emergency room services-A prospective study. J Ment Health Hum Behav. 14.
- Grover S. (2011). State of consultation-liaison psychiatry in India: Current status and vision for future. Indian J Psychiatry. 53:202.
- Bronheim HE, Fulop G, Kunkel EJ, Muskin PR, Schindler BA, Yates WR, et al. (1998). The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. The Academy of Psychosomatic Medicine. Psychosomatics. 39:28-30.
- Clarke DM, Smith GC. (1995). Consultation-liaison psychiatry in general medical units. Aust N Z J Psychiatry. 29:424–432.
- Arolt V, Driessen M, Dilling H. (1997). The Lübeck General Hospital Study. I: Prevalence of psychiatric disorders in medical and surgical inpatients. Int J Psychiatry Clin Pract. 1:207–216.
- Woon LSC, Redzuan NI. (2019). Characteristics of Patients Referred for Consultation-liaison Psychiatry in a Regional Referral Hospital in Malaysia. Malays J Psychiatry. 81–86.
- Wood R, Wand APF. (2014). The effectiveness of consultation-liaison psychiatry in the general hospital setting: a systematic review. J Psychosom Res. 76:175–192.
- Sidana A, Kaur P, Chavan BS, Arun P, Singh GP. (2007). Practice and Pattern of Psychiatry referrals in a tertiary care teaching hospital. J Mental Health and Behaviour. 12:31-37.
- Tekkalaki B, Tripathi A, Arya A, Nischal A. (2017). A descriptive study of pattern of psychiatric referrals and effect of psychiatric intervention in consultation-liaison set up in a tertiary care center. Indian J Soc Psychiatry. 33:165-170.
- Jhanjee A, Kumar P, Srivastava S, Bhatia MS. (2011). A Descriptive Study of Referral Pattern in Department of Psychiatry of A Tertiary Care Hospital of North India.
- Goyal SG, Sagar R, Sharan P. (2017). Sociodemographic profile and psychiatric diagnosis of patients referred to consultation-liaison psychiatric services of general hospital psychiatric unit at a Tertiary Care Center. J Mental Health Hum Behav. 22:45-49.
- Mathur P, Sengupta N, Das N, Bhagabati D. (2015). A study on pattern of consultation liaison psychiatric service utilization in a tertiary care hospital. J Res Psychiatry Behav Sci.
- Grover S, Sarkar S, Avasthi A, Malhotra S, Bhalla A, Varma SK. (2015). Consultation-liaison psychiatry services: Difference in the patient profile while following different service models in the medical emergency. Indian J. Psychiatry. 57:361.
- Murthy RS. (2017). National Mental Health Survey of India 2015–2016. Indian J Psychiatry. 59:21–26.
- Zeller S, Calma N, Stone A. (2014). Effects of a dedicated regional psychiatric emergency service on boarding of psychiatric patients in area emergency departments. West J Emerg Med. 15:1–6.
- De Giorgio G, Quartesan R, Sciarma T, Giulietti M, Piazzoli A, Scarponi L, et al. (2015). Consultation-Liaison Psychiatry—from theory to clinical practice: an observational study in a general hospital. BMC Res Notes. 8:475.
- Lucca JM, Vamsi A, Kurian SJ, Ebi S. (2019). A prospective observational study on psychotropic drug use in non psychiatric wards. Indian J Psychiatry. 61:503.
- Huyse FJ, et al. Consultation-Liaison psychiatric service delivery: results from a European study. Gen Hosp Psychiatry 2001: 23:124–132.
- Yamada K, Hosoda M, Nakashima S, Furuta K, Awata S. (2012). Psychiatric diagnosis in the elderly referred to a consultation-liaison psychiatry service in a general geriatric hospital in Japan. Geriatr Gerontol Int. 12:304–309.
- Gupta N, Sharma P, Meagher D. (2010). Predictors of delayed identification of delirium in a general hospital liaison psychiatry service: A study from North India. Asian J Psychiatr. 3:31–32.