Previous Issues Volume 6, Issue 2 - 2024
Nurses’ Optimal Implementation of Smoking Cessation Intervention: A Single-Institution Experience
Reiko KORI1, Kanji OTSUBO², Hiroki SAKAI², Hiroyuki KIMURA², Tomoyuki MIYAZAWA², Hideki MARUSHIMA², Koji KOJIMA², Masatoshi HARA3, Hisashi SAJI²,*
1Department of Nursing, St. Marianna University School of Medicine, Kawasaki, Japan
²Department of Chest Surgery, St. Marianna University School of Medicine, Kawasaki, Japan
3Division of Cardiology, Department of Internal Medicine, St. Marianna University School of Medicine, Kawasaki, Japan
*Corresponding Author: Hisashi Saji, MD, PhD, Professor, Department of Chest Surgery, St. Marianna University School of Medicine, 2-16-1 Sugao, Miyamae-ku, Kawasaki, Kanagawa 216-8511, Japan; Tel: +81-44-977-8111; Fax: +81-44-976-5792; Email: [email protected]
Received Date: April 29, 2024
Published Date: May 10, 2024
Citation: KORI R, et al. (2024). Nurses’ Optimal Implementation of Smoking Cessation Intervention: A Single-Institution Experience. Mathews J Nurs. 6(2):43.
Copyrights: KORI R, et al. © (2024).
ABSTRACT
Background: Smoking cessation can be taught in many ways, but few studies have examined the effectiveness of smoking cessation interventions following the questions in the tobacco dependence screener (TDS). Aims: This study aimed to establish a base for developing tailored smoking cessation training programs to ensure nurses’ optimal implementation of smoking cessation interventions for patients. Methods: This study extracted and analyzed data, including TDS results, teaching details, and clinical outcomes, from the medical records of patients who visited our smoking cessation clinic from August 2018 to March 2020. Findings: No statistical difference was observed in the mean TDS score, Brinkman index, or mean age between patients who successfully and failed to quit smoking. In brief, 15 successfully quit smoking, whereas 6 failed. The success rate of smoking cessation was higher in the group with a TDS score of ≥8 than in the group with a TDS score of <8 (80.0% vs. 63.6%). Conclusion: Targeted interventions based on patient responses to the TDS may significantly impact the success of smoking cessation than simple advice alone.
The name of the trial register: Institutional Review Board of St. Marianna University School of Medicine
Keywords: Japan, Nurses, Nursing, smoking cessation intervention, the tobacco dependence screener
INTRODUCTION
Tobacco smoking is the leading preventable cause of cancer, cardiovascular diseases, other respiratory diseases, and even premature death worldwide [1,2].
Social awareness remains low although smoking is preventable, and the antismoking movement in Japan is weak compared to that of western countries. Smoking provides a pleasurable feeling, thereby reinforcing an individual to continue such behavior. The behavioral science approach is as important as drug therapy for nonsmoking therapy.
BACKGROUND
Nurses play an important role in motivating smokers to quit [3-6], and the impact of nursing interventions on smoking cessation is extensively documented. Unfortunately, the reliability of patients’ smoking status reports is debatable, and the assessment method remains an issue for all health professionals.
Hence, this study aimed to establish a base for developing tailored training programs to ensure nurses’ optimal implementation of smoking cessation intervention for patients.
THE STUDY
Aims
This study aims to explore the possibility of more effective smoking cessation teaching methods in the future and discover the actual smoking cessation treatment methods in Japan and their present status in our hospital.
Design
Japan’s National Health Insurance (NHI) covered smoking cessation in 2006 and standard nursing procedures for smoking cessation programs were implemented.
This preliminary trial hypothesized that a behavioral model of smoking cessation intervention based on patients’ responses to the Tobacco Dependence Screener (TDS) would have a greater impact on smoking cessation than simple advice alone.
The “not applicable” answers to certain TDS questions might indicate patients’ unawareness. This tendency was particularly strong among patients who were close to the TDS 5-point line.
Therefore, this retrospective study was conducted on outpatients who visited our hospital for smoking cessation. We suggested that the success rate of smoking cessation could be increased by roughly identifying patients’ awareness status using the answered TDS during their first visit and by counseling, emphasizing more on the TDS questions that patients answered as “not applicable.”
The sixth edition of the Standard Procedure for Smoking Cessation Treatment lists examples of specific practices for teaching smoking cessation [7]. However, this standard procedure is not absolute; it is frequently performed flexibly according to the patient despite available policies to guide its use. The ultimate goal is to quit smoking, and the specific content of smoking cessation counseling is left up to the assigned physicians and nurses. Additionally, the knowledge level and interviewing skills regarding smoking cessation guidance varies among physicians and nurses at each facility. For instance, those who passed the certification examinations for certified smoking cessation counselors and specialist counselors in the Japanese Society for Smoking Cessation were evaluated for the specified knowledge and skill levels. However, providing smoking cessation treatment without these qualifications remained possible. Therefore, the content of smoking cessation guidance at each facility greatly varies, and some facilities can maintain a high success rate in smoking cessation, while others cannot. Presenting the specific smoking cessation guidance in response to the answered TDS by the patients would make the smoking cessation guidance easier to understand, thereby providing more practical guidance.
Sample
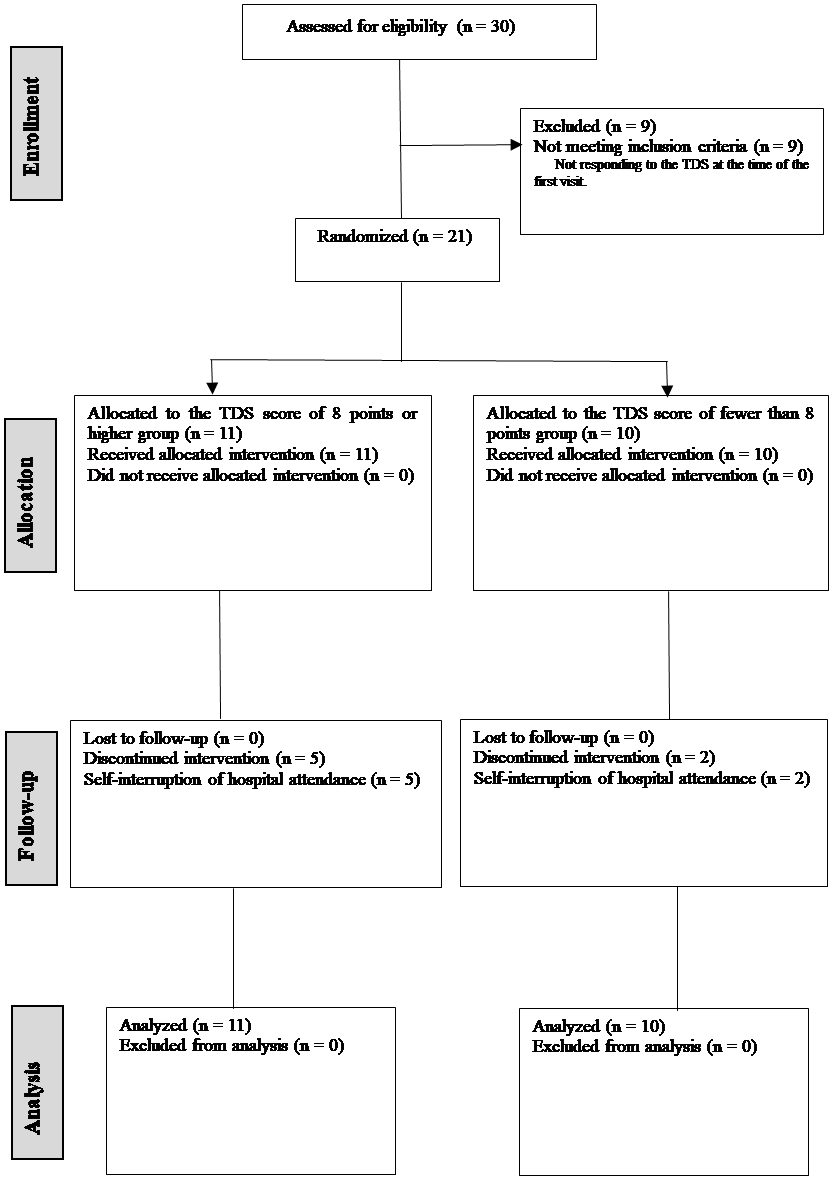
This study reviewed the medical records of 21 patients who visited our hospital for smoking cessation from August 2018 to March 2020 to collate pre-intervention data, which were documented on nurses’ records of smoking status.
Data Collection
Data were collected from the medical records of all 30 patients who visited the smoking cessation outpatient clinic of St. Marianna University Hospital for nicotine dependence treatment from August 2018 to March 2020. Additionally, the intervention status of the nurses and the smoking status of the patients were checked.
The medical record review revealed that 21 of the 30 patients answered the TDS during their first smoking cessation clinic visit. Then, the content of the nurses’ smoking cessation teaching intervention and the success/failure of smoking cessation were retrospectively examined according to the TDS responses.
Data were analyzed according to the hypothesis that patients who answered “not applicable” to TDS questions were less likely aware of these questions and focusing the instructional intervention on these questions would be more effective in helping the patients quit smoking.
Briefing and Screening of the Patients for the Standard Treatment Program for Smoking Cessation
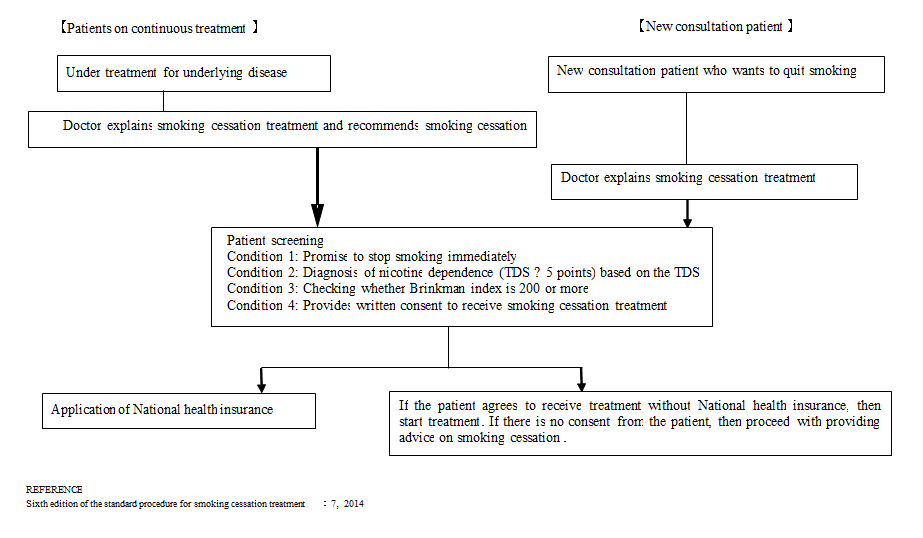
The sixth edition of the Standard Procedure for Smoking Cessation Treatment defines the criteria for screening patients during their initial consultation, as shown in Figure 1 [7].
Figure 1: Explanation and Screening of Smoking Cessation Treatment.
In Japan, the smoking cessation treatment of patients who met these criteria would be covered by NHI. Otherwise, only one-third of the treatment would be covered. Our clinic provides no free smoking cessation treatment; thus, this study only included those who met the above-mentioned conditions.
Standard Treatment Program for Smoking Cessation
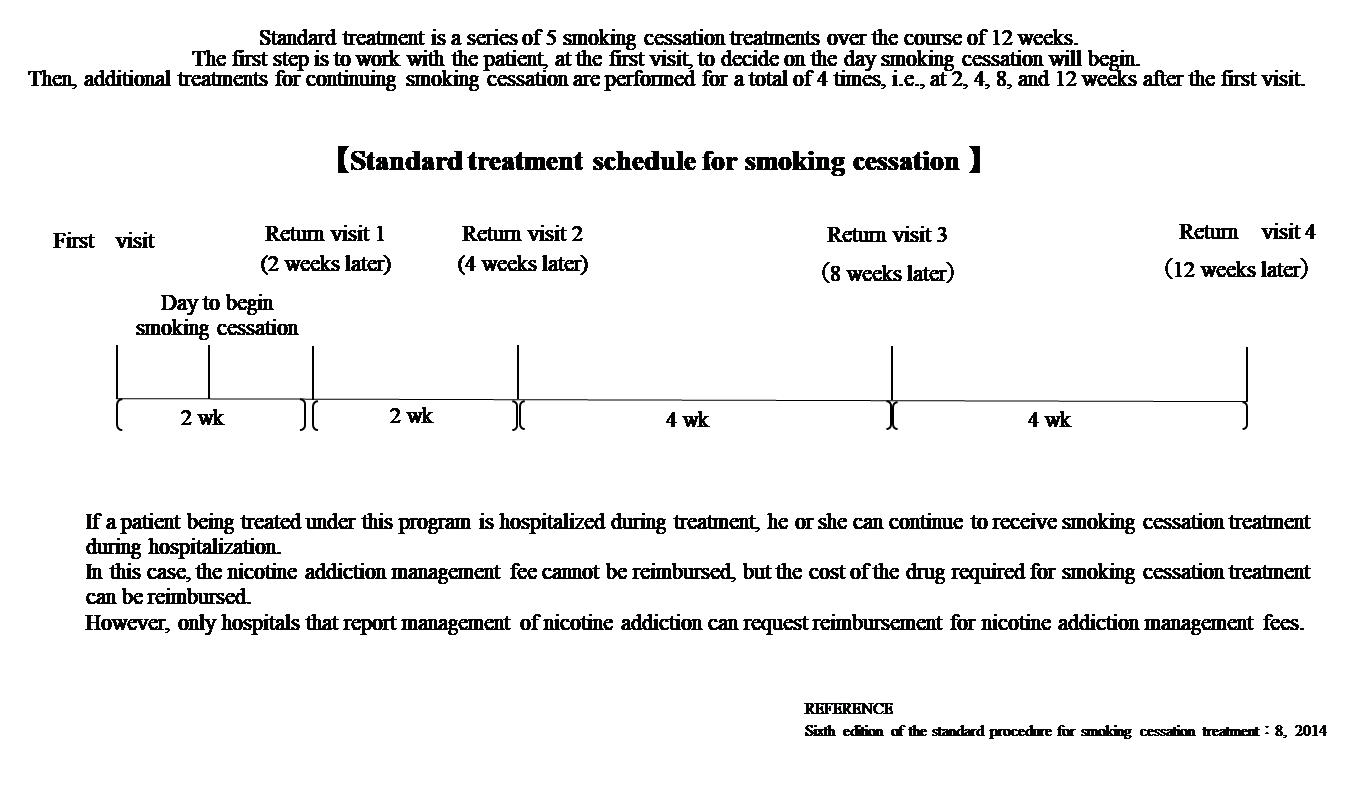
The standard treatment included a series of five smoking treatments for 12 weeks. Initially, we worked with the patient during the first visit to decide when to begin smoking cessation. Then, additional interventions were provided to help the patient continue smoking cessation at 2, 4, 8, and 12 weeks after the first visit (Figure 2). The program continues even with patient hospitalization. Hence, the nicotine addiction management fee cannot be reimbursed, except for the cost of the required drug for smoking cessation. However, only hospitals that report nicotine addiction management can request reimbursement.
Figure 2: Standard Treatment Program For Smoking Cessation.
The Intervention
We applied the sixth edition of the standard procedure and engaged nurses for the smoking cessation program, which comprised five patient visits, including interventions from both physicians and nurses and medications for 12 weeks (Figure 2).
Figure 3: CONSORT diagram for the investigation.
The final analysis included 21 patients.
The nurses’ interventions were conducted in the outpatient consultation room in our hospital. Medical records included patients’ smoking cessation status, smoking cessation medication status and its side effects, the guidance of nurses, and patient responses to questions regarding their concerns and problems.
Patients answered the TDS during the first visit, the physician prescribed and instructed smoking cessation medication, and the nurse provided smoking cessation guidance to the patient.
Only the oral medication varenicline was used as a smoking cessation aid. Nicotine patches were not prescribed, except for patients scheduled to undergo hemodialysis for renal dysfunction. Patients who underwent nephrectomy and had an estimated glomerular filtration rate of <30 and those who quit smoking without any problems even after self-adjusting the medication frequency in the outpatient clinic were consulted and given counseling without prescribing medication.
The patients’ TDS results obtained during the initial consultation were always checked by one of the researchers during each patient visit to understand patient tendencies, their focus, and their concerns before providing guidance.
Ethical Considerations
We attended a training session on ethical guidelines for medical research on human subjects and stored and managed the collected data in a universal serial bus with a password lock to prevent easy access. A correspondence table was created and analyzed with the name and patient ID deleted when extracting personal information from the medical records, and a new case registrant number was added. The collected personal information and the correspondence table will be kept for 5 years after the research’s completion or cessation or 3 years after the last day of reporting the results, such as a presentation at an academic conference, whichever is later. This information will be used only by the university and will not be provided to other research institutions.
Moreover, this study was approved as an observational study using medical information obtained through regular medical care. The information will be disclosed on the institution’s website as ongoing research following the institution’s regulations where the research was conducted, and data will be excluded from the research if patients request refusal of participation.
This study was approved by the institutional review board of the St. Marianna University School of Medicine in Kanagawa, Japan (Accession No. 5214). All patient data remained confidential throughout this research.
Data Analysis
Nurses documented patients’ smoking status and the appropriate interventions in the medical record and nursing care plan.
We investigated the nursing interventions provided in response to patients’ reactions to the TDS. The results were first calculated using the following score distribution based on the hypothesis that patients may not be aware of the content of their “not applicable” responses to the TDS and that intervening in this content may improve the success rate of smoking cessation.
●If a patient answered “yes” and was intervened, the score is 0.
●If a patient answered “yes” and was not intervened concerning the content related to the question, the score is −1.
●If a patient answered “no” and was intervened, the score is +1.
●If a patient answered “no” and was not intervened concerning the content related to the question, the score is −2.
Mann–Whitney’s U test was used to analyze the results obtained from the original score distribution table. Statistical data were analyzed using JMP Pro14.
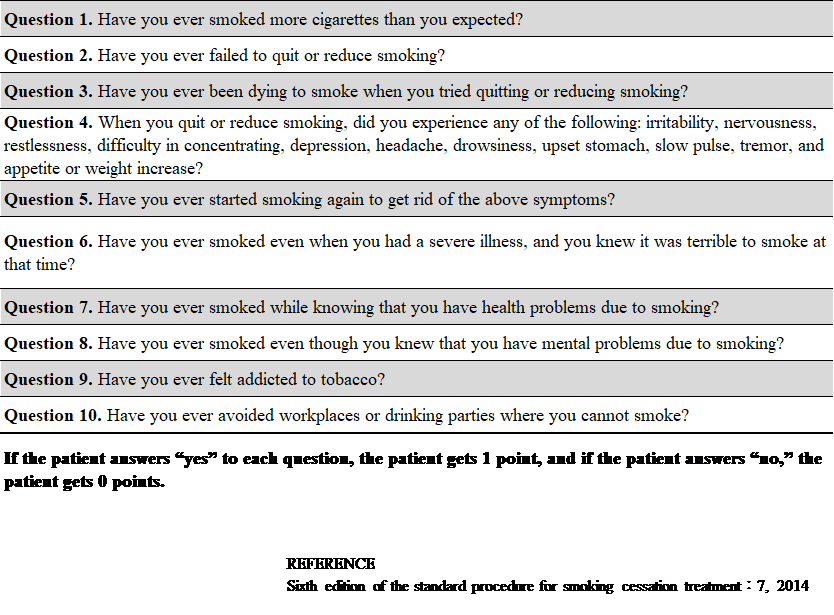
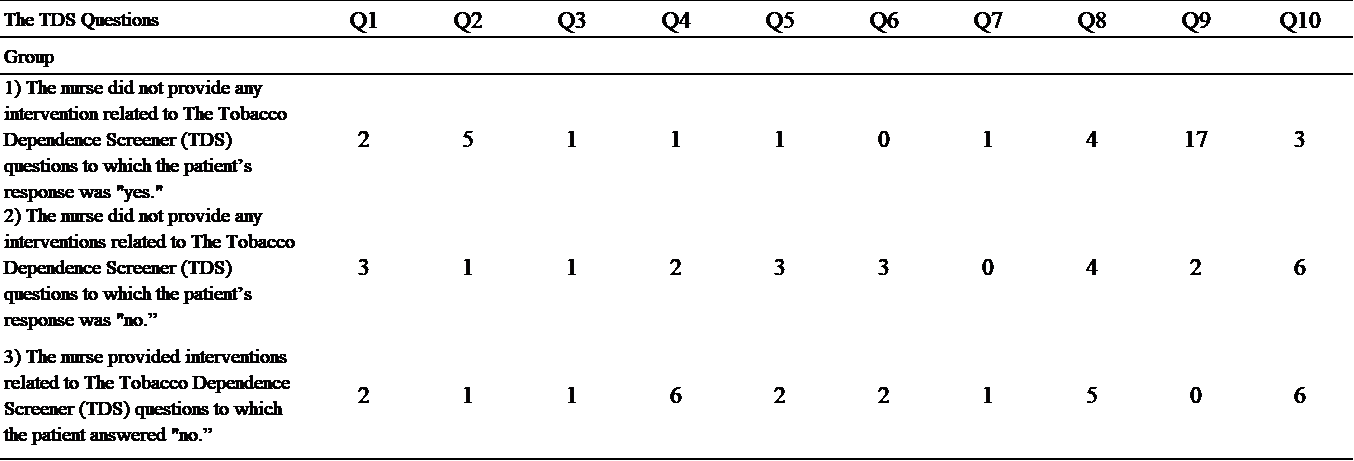
Table 1: Contents of the TDS.
Table 2: Summary of the responses obtained from the TDS and the results of the nurses’ interventions.
Patient responses were obtained upon the first visit; the nurse interventions for each TDS question are presented as the number of interventions performed during the five treatment sessions.
The difference in the amount of nurses’ intervention and the success rate of smoking cessation according to the TDS score was also investigated. We divided the scores by a line of 8 points, which is the middle line of six levels ranging from 5 to 10 points, and analyzed the difference between the group with a TDS score of 8 points or higher and the group with a score of fewer than 8 points for comparison.
Validity and Reliability/Rigor
The TDS, which is used to select patients for insurance coverage, was developed to diagnose nicotine dependence from a psychiatric perspective following the World Health Organization (WHO)’s International Classification of Diseases, 10th Edition (ICD-10) and the American Psychiatric Association’s Guides to the Classification and Diagnosis of Mental Disorders, third and fourth editions (DSM-III-R, DSM-IV). This test was used in the “Survey on Smoking and Health Problems” conducted by the Ministry of Health and Welfare in 1998.
The TDS consists of 10 questions, wherein 1 point is given for “yes” and 0 for “no,” and the total score is calculated. A TDS score of 5 or higher (0–10) indicates nicotine dependence. Its reliability and validity were tested in Japanese subjects. The sensitivity and specificity of this test are 95% and 81%, respectively, using the ICD-10 diagnostic results of the WHO Consolidated International Diagnostic Interview (WHO-CIDI) as the gold standard.
The Fagerström Nicotine Dependence Index (FTND) is a globally known screening test used for physiologically assessing the degree of nicotine dependence. However, the correlation between the Fagerström Tolerance Questionnaire, which is an older version of the FTND, and the ICD-10 is lower than that of the TDS [7]. Table 1 lists 10 TDS questions that were asked on the first visit.
RESULTS/FINDINGS
Of the 30 patients who visited our smoking cessation outpatient clinic during the target period, 9 were excluded because of incorrect TDS acquisition during the first visit. Some of the 21 remaining patients self-interrupted their visits within the course of the program; hence, we considered them to have failed to quit smoking. The 21 included patients consisted of 19 males and 2 females, with a mean age of 66.5 years and a mean pack year of 45. The median TDS score was 7.5 (n = 21). Major comorbidities were listed in the following order: hypertension, angina pectoris, arrhythmia, end-stage renal failure, and malignancy.
In brief, 15 successfully quit smoking, whereas 6 failed. Among them, 16 were long-term heavy smokers. Table 2 summarizes the responses obtained from the TDS and the results of the nurses’ interventions.
Patient’s Response during Smoking Cessation Instruction
Patients tended not to talk considerably about the content of the “no” answers on the TDS but respond positively to the content of the “yes” answers during the smoking cessation guidance. Patients tended to reply “I do not particularly care. I do not think that is true,” when the nurses tried to instruct the patients about the “no” answers on the TDS, making it difficult to intervene. However, these patients claimed that the content of their “no” answers to the TDS was often their obstacle to achieving smoking cessation.
Characteristics of Patients who had Successfully Quit Smoking
The mean age, TDS score, and Brinkman index of patients who successfully quit smoking were 68.5 years, 7.6, and 1046, respectively.
Characteristics of Patients Who had failed to Quit Smoking
The mean age, TDS score, and Brinkman index of patients who failed to quit smoking were 61.6 years, 7.5, and 1088, respectively.
Analysis using A Proprietary Scoring Table
The original scoring distribution analyzed by JMP Pro14 revealed no statistically significant differences. The result analysis for each question revealed varied numbers of “yes” and “no” answers. Hence, testing the results of this original scoring distribution table was deemed inappropriate. The success rate of smoking cessation was higher in the group with a TDS score of ≥8 than in the group with a TDS score of <8 (80.0% vs. 63.6%).
The median number of interventions (number with intervention) in the group with a TDS score of ≥8 was higher in the failure group than in the success group (8.5 vs. 7). Thus, the failure group received more interventions. The median number of interventions (with interventions) in the group with a TDS score of <8 was lower in the failure group than in the success group (6 vs. 7), indicating that the success group received more interventions.
DISCUSSION
Brief Summary
The group with a TDS score of ≥8 had a higher success rate of smoking cessation, despite receiving fewer interventions, possibly because they knew and acknowledged their smoking status.
Conversely, the group with a TDS of <8 did not have a firm grasp of their smoking status. Therefore, they needed more interventions to successfully quit smoking. The results suggest that increasing the amount of intervention by focusing on what patients answered “No” to the TDS may increase the success rate of smoking cessation in patients whose TDS is close to the 5-point line. Additionally, interventions that help patients become aware of their current smoking status and problems may provide a shortcut to successful smoking cessation.
Comparison with Previous Studies
Reports on the association between interventions based on patient responses to the TDS and success rates of smoking cessation remained tremendously limited. The current study first allocated scores by scoring according to a hypothesis to understand patient tendencies. However, this score allocation was not based on previous studies; hence, a personal bias based on how the authors felt from their usual interventions may be possible. The results may change if the study is reconducted using this method with a more significant number of patients.
Possible Explanations and Implications
Our study results suggest that the success rate of smoking cessation can be increased using the TDS scores calculated from patients’ answers during their first visit to roughly determine the degree of their awareness, and by paying attention to the TDS questions answered as “not applicable,” to provide guidance and intervention.
LIMITATIONS
One study limitation includes the small sample size. Minor differences may become significant by increasing the sample size in the future; thus, the results will differ from the present results. However, the most important thing is that the magnitude of the effect of our smoking cessation guidance is returned to the patients. This study is the first step in understanding patients’ attitudes toward smoking cessation and creating a concrete roadmap for devising interventions.
CONCLUSION
An intervention focusing on the TDS questions to which the patients answered “no” may be effective. Therefore, this intervention may be one of the teaching methods that can potentially increase the success rate of smoking cessation. The results of this smoking cessation teaching method are the most significant achievement (new fact) of this research. Further research is necessary to clarify this issue.
Key points
・This study identified specific points of focus when providing smoking cessation guidance and a more effective intervention program.
・The results suggest that increasing the amount of intervention by focusing on what patients answered “No” to the TDS may increase the success rate of smoking cessation in patients who’s TDS is close to the 5-point line.
・Conscious intervention on TDS questions to which patients answered “no” may help identify barriers to successful smoking cessation.
・The intervention method examined in this study may be one of the teaching programs that may increase the success rate of smoking cessation.
Conflict of Interest Statement
No conflict of interest has been declared by the authors.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
I would like to express my sincere gratitude to Professor Hisashi Saji of the Department of Chest Surgery for his enthusiastic guidance throughout the study. I want to express my sincere gratitude to Assistant Professor Masanori Hirose of the Department of General Medicine for his excellent cooperation in analyzing the survey. English editing assistance was provided by Crimson Interactive Pvt., Ltd.
Clinical Trial Registration Number and name of trial register
The institutional review board of the St. Marianna University School of Medicine in Kanagawa, Japan approved this study (Accession No. 5214). All patient data remained confidential throughout this research.
REFERENCES
- Choi SH, Kim YH. (2016). Factors affecting Korean registered nurses’ intention to implement smoking cessation intervention. Osong Public Health Res Perspect. 7(1):63-70.
- Froelicher ES, Kozuki Y. (2002). Theoretical applications of smoking cessation interventions to individuals with medical conditions: Women’s initiative for nonsmoking (WINS)-part III. Int J Nurs Stud. 39(1):1-15.
- Percival J, Bialous SA, Chan S, Sarna L. (2003). International efforts in tobacco control. Semin Oncol Nurs 19(4):301-308. Rice VH, Stead LF. (2008). Nursing interventions for smoking cessation. Cochrane Database Syst Rev. 1:CD001188.
- Chaney SE, Sheriff S. (2012). Evidence-based treatments for smoking cessation. Nurse Pract. 37(4):24-31.
- Sarna LP, Bialous SA, Kraliková E, Kmetova A, Felbrová V, Kulovaná S, et al. (2014). Impact of a smoking cessation educational program on nurses’ interventions. J Nurs Scholarsh. 46(5):314-321
- Node K, Iida M, Ebina T, Saku K, Satoh K, Takahashi Y, et al. (2014). Sixth edition of the Standard Procedure for Smoking Cessation Treatment. Japan: The Japanese Circulation Society, the Japan lung cancer society: Japanese Cancer Association, & The Japanese Respiratory Society.