Previous Issues Volume 9, Issue 8 - 2024
New Surgical Approach to Carpus Callosum Agenesis with Intractable Seizure: Subdural Peritoneal Shunt
Mohammad Ali Fazeli1,*, Malous Emadzadeh2, Mariam Tahmasb Mirza3, Fatemeh Valipoori Goodarzi4
1Functional neurosurgery research center, Shohada Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2ICORD Research Center, Department of Medicine, Division of Surgery, University of British Columbia, Canada
3,4University of Tehran, Tehran, Iran
*Corresponding Author: Dr. Mohammad Ali Fazeli, Functional Neurosurgery Research Center, Shohada Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran, Phone No: 00989123176146, Email: [email protected]
Received Date: July 12, 2024
Published Date: September 20, 2024
Citation: Fazeli MA, et al. (2024). New Surgical Approach to Carpus Callosum Agenesis with Intractable Seizure: Subdural Peritoneal Shunt. Mathews J Case Rep. 9(8):180.
Copyrights: Fazeli MA, et al. (2024).
ABSTRACT
Agenesis of corpus callosum is the most common cerebral malformation’s diagnosis is based on brain imaging. It is most often asymptomatic. Hyperhidrosis can be part of his clinical feature. We present the case of a33 year old patient, unemployed, with a history of simple partial epilepsy and severe headache. He consulted for sense of right hemiparesis with sweating attacks. The defect was identified during the adulthood period by brain computed tomography scan. However, he did not present any craniofacial or non-cerebral malformation suggestive of a congenital syndrome. Furthermore, he showed no neuropsychiatric disorder or intellectual disability during his early childhood. He complained of frequent right partial seizure even with maximum dose of anti-elliptic drug. The patient underwent subdural peritoneal shunting and after 48 hours efficacy of shunting was significant. To describe a surgical technique and to report using efficacy of subdural peritoneal shunts for corpus callosum agenesis We describe the considerations, and outcomes related to this technique.
Keywords: Corpus Callosum Agenesis, Hyperhidrosis, Subdural Peritoneal Shunt.
INTRODUCTION
The corpus Callosum (CC), the major commissural in the brain, is crucial for inter-hemispheric incorporation of sensory, motor, and higher-order cognitive information. Corpus Callosum Agenesis(CCA)is the most common cerebral malformations. It can be symptomatic or asymptomatic. Diagnosis is based on imaging brain. Clinical features are variable, they may include mental retardation, more or less moderate, seizures, "out control" behavior, facial dysmorphism and hyperhidrosis. Treatment is only symptomatic. We report the case of CCA revealed at adulthood by hyperhidrosis attacks and a history of simple partial epilepsy. He complained of frequent right partial seizure even 5-10 times a week and severe headache even with maximum dose of anti-elliptic drug. The patient underwent subdural peritoneal shunting with dramatic response in form of seizure attacks control and headache recovery.
DISCUSSION
Agenesis of the corpus Callosum (AgCC) is an uncommon brain malformation that can happen isolated or in connection with other anatomical disorders as part of a complex congenital syndrome [1]. The defect is "complete" when total absence of the corpus Callosum (CC) happens or "partial" when only firm areas of the structure are made.
Despite the gross anatomical consequences of this disorder, the spectrum of neurological manifestations detected in those with AgCC varies from severe intellectual disability to normal intelligence [2-4]. However, even in patients with isolated AgCC and no apparent neurological deficit, subtle neuropsychological variations may happen as the cognitive demand rises with age [5,6].
Therefore, a long-term follow-up by sufficient neuropsychological screening is essential for all cases of AgCC and "normal" intellectual quotient (IQ). Unfortunately, because of the scarcity of this malformation, information of the neurological and cognitive features of AgCC is constrained among physicians, which may cause a late identification of neurocognitive changes and to a delayed founding of rehabilitative strategies designed to improve compensatory functions in affected patients.
Here, we describe the case of a 33 years old with isolated total AgCC and obvious grossly intact general intelligence. Our study targeted a new surgical approach in AgCC in which seizures can be controlled with minimal complications instead of conventional surgery.
CASE PRESENTATION
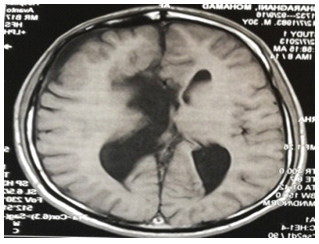
A 33-year-old man attended our center to receive a follow-up medications examination because his wife had stated that he was diagnosed as having AgCC during the neonatal period and complained of his frequent seizure and headache. Thus, a computed tomography (CT) scan and MRI of his brain was performed which confirmed the diagnosis. Also, no evidence of visual or hearing impairment was detected. His pattern of postnatal growth and neurocognitive development was normal. Furthermore, he did not show any neurological sign, behavioral or psychiatric disorder, or intellectual disability during his early childhood and school age. The rest of his past medical history was relevant only for hyperhidrosis. At the age of 30 he was subjected to a control magnetic resonance imaging (MRI) of his brain that showed total AgCC, as well as enlargement of the lateral ventricles with dilated occipital horns (colpocephaly; Figure 1). However, he did not present any clinical data of intracranial hypertension. His chief complaint was frequent partial seizure affecting right limb predominantly with movement and sensory involvement last for 1 minute repeating averagely 5-10 times a week with maximum dose of anti-elliptic drugs.
Figure 1. Brain magnetic resonance imaging images of the clinical case. Sagittal (upper panels) and transversal (lower panels) T1-weighted brain magnetic resonance imaging images showing total agenesis of the corpus callosum and enlargement of the occipital horns of the lateral ventricles.
During the medical examination he was alert, aware, oriented, and asymptomatic. His language was partially fluent, and his posture was normal with no abnormal movements.
He was able to follow simple commands and to name objects. He did not present evidence of any apraxia or agnosia. A physical examination revealed normal gait, and no alterations in cranial nerve reflexes, muscle strength, deep tendon reflexes, and plantar reflexes. An examination of the cerebellum did not show any abnormality, and no clinical features of intracranial hypertension and meninges were observed., as well as electrolyte and vitamin panel were normal.
Finally, non-pharmacological management was prescribed, and he was scheduled for subdural peritoneal shunt insertion at our center figure 2. The legal guardian of the patient provided written informed consent for the publication of the case.
Post operation the patient feels better obviously, his headache recovered and partial seizures significantly decreased to one attack in a period of 4 months even though drug dose was diminished. Other vagus senses like blushing and agitation healed.
CONCLUSION
The CCA is a common malformation. It may be asymptomatic or reveled by a highly polymorphic and non-specific clinical feature. It should be researched in prenatal, postnatal and even in adulthood. Hyperhidrosis attacks without obvious underlying pathology should consider this diagnosis. Maybe another mechanism rather than internal hydrocephalus like progressive external hydrocephalus and impaired dynamic of CSF circulation in CCA lead to intractable seizure that can be handled by subdural peritoneal shunt. Replacing such a less invasive surgery compared to more invasive surgical approach can be a great success if be proven. In point of my view progressive external hydrocephalus as a source for intractable seizure in CCA beside structural malformation should be addressed surgically.
REFERENCES
- Palmer EE, Mowat D. (2014). Agenesis of the corpus callosum: A clinical approach to diagnosis. Am J Med Genet Part C Semin Med Genet. 166(2):184-197.
- Taylor M, David AS. (1998). Agenesis of the corpus callosum: A United Kingdom series of 56 cases. J Neurol Neurosurg Psychiatry. 64(1):131-134.
- Moutard ML, Kieffer V, Feingold J, Lewin F, Baron JM, Adamsbaum C, et al. (2012). Isolated corpus callosum agenesis: A ten-year follow-up after prenatal diagnosis (How are the children without corpus callosum at 10 years of age?). Prenat Diagn. 32(3):277-283.
- des Portes V, Rolland A, Velazquez-Dominguez J, Peyric E, Cordier MP, Gaucherand P, et al. (2018). Outcome of isolated agenesis of the corpus callosum: A population-based prospective study. Eur J Paediatr Neurol. 22(1):82-92.
- Brown WS, Paul LK. (2019). The Neuropsychological Syndrome of Agenesis of the Corpus Callosum. J Int Neuropsychol Soc. 25(3):324-330.
- Lábadi B, Beke AM. (2017). Mental State Understanding in Children with Agenesis of the Corpus Callosum. Front Psychol. 8:94.
.png)