Previous Issues Volume 9, Issue 7 - 2024
Necrotizing Fasciitis Post-Uncomplicated Colonoscopy: A Case Report
Ali Mehri1, Mohammad hossein Taherynejad2, Zahra Kargar1, Parnian Eghbali2, Abbas Abdollahi1, Mohammad Etezadpour1,*
1Endoscopic and Minimally Invasive Surgery Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
2Student Research Committee, Mashhad University of Medical Sciences, Mashhad, Iran
*Corresponding author: Mohammad Etezadpour, Endoscopic and Minimally Invasive Surgery Research Center, Mashhad University of Medical Sciences, Mashhad, Iran, Tel: +989355013611, Email: [email protected]
Received Date: June 01, 2024
Published Date: August 05, 2024
Citation: Mehri A, et al. (2024). Necrotizing Fasciitis Post-Uncomplicated Colonoscopy: A Case Report. Mathews J Case Rep. 9(7):174.
Copyrights: Mehri A, et al. © (2024).
ABSTRACT
Necrotizing fasciitis is a rare life-threatening infection with significant mortality which leads to necrosis of subcutaneous tissue. The urgency of the patient's condition along with the high rate of misdiagnosis makes the early diagnosis of necrotizing fasciitis a challenge. This case describes necrotizing fasciitis of the thigh as a rare complication of colonic perforation following an uncomplicated colonoscopy. In this case, we highlight the importance of taking a thorough past medical history, paired with physical examination as a novel key to diagnosing necrotizing fasciitis in this unique case. Furthermore, we reviewed the literature centering on such complications following colonoscopy.
Keywords: Necrotizing Fasciitis, Colonoscopy, Rare, Complications.
ABBREVIATIONS
NF: Necrotizing Fasciitis; CRP: C-reactive Protein; VBG: Venous Blood Gas; PCO2: Pressure of Carbon Dioxide; HCO3: Bicarbonate Concentration; ABG: Arterial Blood Gas; NSAIDs: Non-Steroidal Anti-Inflammatory Drugs; LRINEC: Laboratory Risk Indicator for Necrotizing Fasciitis.
INTRODUCTION
Necrotizing fasciitis (NF) is an urgent surgical condition that causes muscle fascia and subcutaneous tissue necrosis due to intrusive skin and soft tissue infections [1].
This acute infection transpires rapidly through the fascial plane with low blood supply and causes secondary infection in the under and overlying skin, soft tissue, and muscle, as well as causing symptoms of sepsis such as fever, tachycardia, and disorientation [2-4].
The epidemiology of NF depends on the area of the world. In the United States, NF affects about 0.4 per 100,000 people annually. Moreover, NF has a significant mortality rate ranging from 29% to 100% [1,5-7].
Based on microbiology, NF is categorized into polymicrobial and monomicrobial. Staphylococcus aureus and Streptococci are the main cause of these infections. Additionally, polymicrobial NF is sustained by both aerobic and anaerobic bacteria [1, 8].
Most of the patients usually have a background of being post-surgical, history of diabetes, a history of consumption of alcohol, liver cirrhosis, immune suppression, and heart disease [1,9].
According to the high mortality and morbidity rate of NF, early diagnosis, emergency surgical debridement, and broad-spectrum antibiotic therapy is of great importance in decreasing the mortality rate in patients [9,10]. Patient history plays a vital role in early diagnosis and possible suspicion of NF. To date, only a few case reports exist of NF after endoscopic procedures. In this study, we highlight the importance of using the patient's history and physical examination to diagnose NF.
CASE DESCRIPTION
A 60-year-old female patient presented to the emergency department with a chief complaint of acute thigh pain. The pain began 2 days ago in the lateral region of the right thigh and has progressively intensified, becoming intolerable, prompting her visit to the ER. She has no significant past medical history and denies any history of alcohol, tobacco, or illicit drug use. She reports no family history of diseases or prior surgical interventions.
The patient mentioned chronic constipation persisting for over two months, for which she underwent a colonoscopy 2 weeks ago. The colonoscopy revealed a large pedunculated polyp measuring 4 centimeters, located 12 centimeters from the anal verge. Histopathological analysis from a biopsy of the polyp reported a sessile serrated adenoma with low-grade dysplasia, necessitating tumor resection by colonoscopy. Five days after the initial colonoscopy, she underwent a second colonoscopy for polyp resection. Both procedures were reported as uneventful.
Upon initial evaluation in the emergency department, the patient presented with vital signs of a blood pressure measuring 95/80 mmHg, a pulse rate of 122 beats per minute, a respiratory rate of 18 breaths per minute, and a body temperature of 38 degrees Celsius. Cardiopulmonary examination revealed a regular rate and rhythm without murmurs, rubs, or gallops. Auscultation of the lung fields revealed clear bilateral air entry, and abdominal examination indicated a soft, non-tender, non-distended abdomen with normal bowel sounds and the absence of organomegaly.
Detailed examination of the lower extremities identified erythematous swelling in the posterior region of the right thigh upon visual inspection. Palpation of the lesion revealed tenderness without crepitation, and no pain was elicited in the upper or lower joints.
Given the patient's shock status, she was admitted for further diagnostics and primary resuscitation.
Laboratory analyses unveiled a leukocyte count of 11.2/uL (comprising 89.8% neutrophils, 1.8% mixed, and 8.4% lymphocytes), a platelet count of 200 × 10^3, hemoglobin concentration of 6.5 gm/dL, hematocrit level of 21%, and a C-reactive protein (CRP) level of 188.3 mg/L. Urinalysis displayed positive results for glucose and negative for blood. Venous blood gas (VBG) analysis demonstrated a pH of 7.51, partial pressure of carbon dioxide (PCO2) at 25 mmHg, and bicarbonate concentration (HCO3) of 19.9 mmol/L. Arterial blood gas (ABG) analysis indicated a pH of 7.24, pCO2 of 30.2 mmHg, and HCO3 of 12.4 mmol/L.
The patient underwent an emergent examination under anesthesia in the operating room. Utilizing sterile techniques, including prepping and draping, and administering general anesthesia, a midline incision was performed from the navel to the pubis. Intraoperative exploration revealed an absence of free fluid or pathological abnormalities in the small intestine and colon. Notably, an abscess containing purulent material was identified involving the right and posterior aspects of the rectum.
The abscess within the pelvic cavity underwent drainage and lavage. Given the determination that the abscess resulted from a microscopic perforation, the decision was made to perform a sigmoid loop colostomy.
To facilitate drainage, a Pitzer drain and a Nelaton drain were inserted into the abscess cavity, exiting from the right side of the abdomen. Subsequently, the layers of the abdominal wall were closed in their anatomical positions.
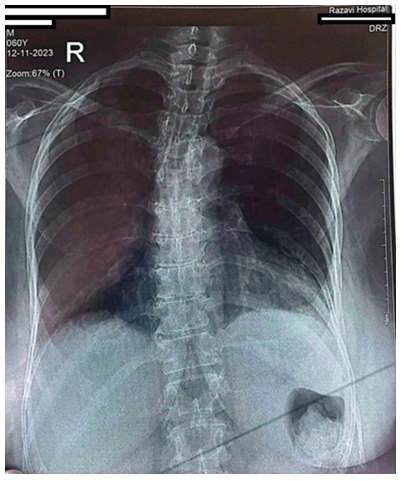
Figure 1. Chest X-ray of the patient (PA view).
Figure 2. Right thigh X-ray. Signs of free air beneath the fascia are apparent.
DISCUSSION
NF is an infectious disease process with frequent clinical findings such as pain, swelling, and erythema, while fever appears only in 40% of patients. In cases with a late diagnosis, bullae, skin necrosis, crepitus, and septic shock may be present [10]. Most of these organisms are gas-forming and cause palpable crepitus, and emphysema which may be shown on plain radiographs [11]. In some cases, especially post-surgery patients, NF is not initially diagnosed and patients are missed due to the lack of symptoms such as fever, caused by the use of non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics, and steroids [10]. In studies conducted by Goh et al and Wong et al. in a large published series, NF was missed or misdiagnosed initially in 75% and 85%-100% of cases, respectively [12,13].
For this purpose, in 2003, Wong et al. conducted a study in risk stratification patients for distinguished NF with other severe soft tissue infections by the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) scoring system. However, the significant difference in the validation results of the LRINEC scoring system, which led to a new scoring system as modified LRINEC (m-LRINEC) with high sensitivity and specificity [13-15].
The diagnosis of NF is principally clinical. Although lab tests and imaging are helpful, a definitive diagnosis is by exploratory surgery. Imaging like magnetic resonance imaging (MRI) and computed tomography (CT) scans have high sensitivity (93% and 80%, respectively) in diagnosing NF. However, Kehrl T. reported that NF was missed following the use of MRI and CT scans [16,17]. Moreover, the cause of infection can be identified in nearly 75% of patients admitted with NF through preoperative, intraoperative sampling and blood culture. Unlike blood cultures, which are positive in 25% of cases, cultures taken from the site of injury during surgical debridement are positive in 80% of cases [18,19]. Therefore, it should be considered that laboratory tests or imaging should not prevent surgical intervention as soon as possible [1,11].
In this study, the infection's abdominal cavity was the origin, while its symptoms were solely in the right thigh. As there was no sign of any penetrating injury, it's likely due to new manifestations from her last colonoscopy procedure. In the colonoscopy procedure, the air blows through the small tube into the colon and could cause iatrogenic perforation and spread air into the retroperitoneum. This perforation is an unusual way to transport the air and microbes in the intestine down through the inguinal canal and cause NF of the thigh [20,21].
NF in the lower limb following perforation of the bowel is scarce, and only a handful of related cases have been reported previously. The causes of bowel perforation have been mentioned so far in the case reports, including colon cancer, diverticulitis, using steroids, and trauma [11,22-25].
The study conducted by Sablone et al. reported a 59-year-old male with NF involving the right thigh after a colonoscopy procedure. The patient's symptoms started soon after returning home. Although the diagnosis of this patient was correct, the timing of the treatment was not appropriate and the patient died due to septic shock [26]. Lonie et al. reported in an 87-year-old female with ulcerative colitis was admitted with septic shock and developed left leg pain following a colonoscopy after 7 days. By taking a detailed history, physical examination, and using imaging and lab tests, the clinical diagnosis of NF was made. She was immediately treated with intravenous fluid resuscitation, inotropic support, empiric antibiotics therapy, and urgent surgical debridement [5].
A study conducted by Chae et al. illustrated a 66-year-old man with a diabetes history, underwent colonoscopic polypectomy. After 24 hours, he felt abdominal pain which was under-treated with a diagnosis of NF based on history taking and CT-scan findings. Unfortunately, the patient died after supportive care and three sessions of surgical debridement [27].
The common feature of all these studies centers in taking a detailed history from the patients. The high rate of misdiagnosis of NF as well as life-threatening conditions has prompted, history-taking as the most valuable and gold tool along with other diagnostic ways.
In our case, the diagnosis was correctly made based on a detailed medical history, which included a colonoscopy 2 weeks prior, followed by an unexplained development of right thigh pain. After the patient was promptly diagnosed before the patient's condition worsened and presented at the emergency department with symptoms of septic shock or toxic state, prompt treatments and supportive care were carried out, and fortunately, the patient's condition improved. As shown, neglecting to mention colonoscopy in the patient's medical history could have led to a misdiagnosis and lack of suspicion for NF.
CONCLUSION
NF may develop after colonoscopy, even if it appears uncomplicated, especially in patients with positive risk factors. Therefore, physicians must pay attention to the possibility of NF as one of its complications by a taking detailed history.
ACKNOWLEDGEMENTS
We would like to thank the staff of the Endoscopic and Minimally Invasive Surgery (EMIS) Research Center at Ghaem Hospital for their outstanding support.
AUTHOR CONTRIBUTIONS
AM: Writing – original draft, Writing – review & editing
MHT: Writing – original draft
PE: Writing – original draft
AA: Supervision
ME: Resources
CONSENT STATEMENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
CONFLICT OF INTEREST DECLARATIONS
The authors declare no conflicts of interest.
REFERENCES
- Wallace HA, Perera TB. (2024). Necrotizing Fasciitis. In: StatPearls. StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC. Treasure Island (FL), USA.
- Kim YH, Ha JH, Kim JT, Kim SW. (2018). Managing necrotising fasciitis to reduce mortality and increase limb salvage. J Wound Care. 27(Sup9a):S20-S27.
- Lange JH, Cegolon L. (2018). Comment on: Early clinical manifestations of vibrio necrotising fasciitis. Singapore Med J. 59(8):449.
- Puvanendran R, Huey JC, Pasupathy S. (2009). Necrotizing fasciitis. Can Fam Physician. 55(10):981-987.
- Lonie S, Rozen WM, Seifman M. (2019). Necrotizing fasciitis following colonoscopy in the setting of ulcerative colitis. ANZ J Surg. 89(11):e546-e547.
- Fernando SM, Tran A, Cheng W, Rochwerg B, Kyeremanteng K, Seely AJE, et al. (2019). Necrotizing Soft Tissue Infection: Diagnostic Accuracy of Physical Examination, Imaging, and LRINEC Score: A Systematic Review and Meta-Analysis. Ann Surg. 269(1):58-65.
- Fais P, Viero A, Viel G, Giordano R, Raniero D, Kusstatscher S, et al. (2018). Necrotizing fasciitis: case series and review of the literature on clinical and medico-legal diagnostic challenges. Int J Legal Med. 132(5):1357-1366.
- Heijkoop B, Parker N, Spernat D. (2019). Fournier's gangrene: not as lethal as previously thought? A case series. ANZ J Surg. 89(4):350-352.
- Khamnuan P, Chongruksut W, Jearwattanakanok K, Patumanond J, Yodluangfun S, Tantraworasin A. (2015). Necrotizing fasciitis: risk factors of mortality. Risk Manag Healthc Policy. 8:1-7.
- Yiasemidou M, Majumder S, Basheer M. (2017). Necrotising fasciitis after laparoscopic rectal cancer surgery. Ann R Coll Surg Engl. 4(99):e113-e114.
- Wiberg A, Carapeti E, Greig A. (2012). Necrotising fasciitis of the thigh secondary to colonic perforation: the femoral canal as a route for infective spread. J Plast Reconstr Aesthet Surg. 65(12):1731-1733.
- Goh T, Goh LG, Ang CH, Wong CH. (2014). Early diagnosis of necrotizing fasciitis. Br J Surg. 101(1):e119-e125.
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. (2003). Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 85(8):1454-1460.
- Wu H, Liu S, Li C, Song Z. (2021). Modified Laboratory Risk Indicator for Necrotizing Fasciitis (m-LRINEC) Score System in Diagnosing Necrotizing Fasciitis: A Nested Case-Control Study. Infect Drug Resist. 14:2105-2112.
- Hoesl V, Kempa S, Prantl L, Ochsenbauer K, Hoesl J, Kehrer A, Bosselmann T. (2022). The LRINEC Score-An Indicator for the Course and Prognosis of Necrotizing Fasciitis? J Clin Med. 11(13):3583.
- Kehrl T. (2014). Point-of-care ultrasound diagnosis of necrotizing fasciitis missed by computed tomography and magnetic resonance imaging. J Emerg Med. 47(2):172-175.
- Gan RK, Sanchez Martinez A, Abu Hasan MA, Castro Delgado R, Arcos González P. (2023). Point-of-care ultrasonography in diagnosing necrotizing fasciitis-a literature review. J Ultrasound. 26(2):343-353.
- Gauzit R. (2006). Infections cutanées graves: définitions, caractéristiques cliniques et microbiologiques [Necrotizing skin and soft tissue infections: definitions, clinical and microbiological features]. Ann Fr Anesth Reanim. 25(9):967-970.
- Bakleh M, Wold LE, Mandrekar JN, Harmsen WS, Dimashkieh HH, Baddour LM. (2005). Correlation of histopathologic findings with clinical outcome in necrotizing fasciitis. Clin Infect Dis. 40(3):410-414.
- Haemers K, Peters R, Braak S, Wesseling F. (2013). Necrotising fasciitis of the thigh. BMJ Case Rep. 2013:bcr2013009331.
- Sablone S, Lagouvardou E, Cazzato G, Carravetta F, Maselli R, Merlanti F, et al. (2022). Necrotizing Fasciitis of the Thigh as Unusual Colonoscopic Polypectomy Complication: Review of the Literature with Case Presentation. Medicina (Kaunas). 58(1):131.
- Haemers K, Peters R, Braak S, Wesseling F. (2013). Necrotising fasciitis of the thigh. BMJ Case Rep. 2013:bcr2013009331.
- Sato K, Yamamura H, Sakamoto Y, Morohashi H, Miura T, Yoshikawa T, et al. (2018). Necrotizing fasciitis of the thigh due to penetrated descending colon cancer: a case report. Surg Case Rep. 4(1):136.
- Chan CC, Williams M. (2013). Fournier gangrene as a manifestation of undiagnosed metastatic perforated colorectal cancer. Int Surg. 98(1):43-48.
- Nowicki J, Rego M, Dean NR. (2019). A case report of a sub-clinical necrotising lower limb infection secondary to pelvic anastomotic leak and chronic corticosteroid use. JPRAS Open. 21:14-18.
- Sablone S, Lagouvardou E, Cazzato G, Carravetta F, Maselli R, Merlanti F, et al. (2022). Necrotizing Fasciitis of the Thigh as Unusual Colonoscopic Polypectomy Complication: Review of the Literature with Case Presentation. Medicina (Kaunas). 58(1):131.
- Chae MK, Shin SY, Kwak MS, Yoon JY, Kim HI, Cha JM. (2021). Fatal Necrotizing Fasciitis Following Uncomplicated Colonoscopic Polypectomy: A Case Report. Clin Endosc. 54(2):280-284.
.png)