Previous Issues Volume 6, Issue 4 - 2024
Living in Isolation: A Thematic Analysis of COVID-19 Patient Experiences, Perceptions and its Literature Review
Ubaid Ullah Shah1, Tooba khan2, Azhar Wahab3, Sayed Anwar Ahmad4, Muhammad Nouman5, Shahan Ur Rabi6, Muhammad Yaqoob7, Irum Hazrat8, Furqan Ul Haq9,*
1Lecturer Peshawar Medical College, Pakistan
2Final Year BDS, Peshawar Dental College, Pakistan
3South Infirmary Victoria Hospital Cork, IRL, Ireland
4Training Medical Officer, King Edward Medical University, Lahore, Pakistan
5Department of Internal Medicine, Khyber Teaching Hospital, Peshawar, Pakistan
6House Officer PIMC Peshawar, Pakistan
7Medical Officer Kuwait Teaching Hospital, Pakistan
8Kuwait Teaching Hospital, Kuwait
9Department of Radiation Oncology, Shaukat Khanum Hospital Peshawar, Pakistan
*Corresponding author: Furqan Ul Haq, Department of Radiation Oncology, Shaukat Khanum Hospital Peshawar, Pakistan, Email: [email protected]
Received Date: November 20, 2024
Published Date: December 27, 2024
Citation: Shah UU, et al. (2024). Living in Isolation: A Thematic Analysis of COVID-19 Patient Experiences, Perceptions and its Literature Review. Mathews J Nurs. 6(4):53.
Copyrights: Shah UU, et al. © (2024).
ABSTRACT
Background: Coronavirus disease 2019 (COVID-19) has not only placed an unprecedented strain on healthcare systems worldwide, but has also caused irreparable physical and psychological damage to those infected. It is essential to understand the disease process and psychological experience of patients with COVID-19, to provide them with efficacious psychological guidance and interventions. This qualitative systematic review sought to explore the experience of COVID-19 patients. Methods: A qualitative study including COVID-19 patients who experienced isolation in Peshawar was conducted from 1st Feb, 2021 to 15th March, 2021. It included 20 males of mean age around 20-60. Audio/telephonic interviews were conducted based on a well-structured Questionnaire comprising seven questions, a copy of which is attached below. Study design: A phenomenological qualitative study using in-depth interviews. Results and Conclusion: Worldwide the pandemic had caused the social and personal lives of human beings to change drastically, the patients initially had negative responses and thoughts regarding isolation in the first week, once time passed, they got used to it and response changed from negative to positive responses in a short time. Psychologically about one third of patients had developed anxiety, depression and hopelessness. Patients had fear of progression of disease but slowly and gradually they got used to it and they developed certain ways of keeping themselves busy such as in tele education and socializing with friends on different social applications using the internet.
Keywords: COVID-19, Patient Isolation, Perception, Social Isolation, Thematic Analysis, Pandemic Response, Psychological Effects, Mental Health, Emotional Impact, Public Health, Pandemic Response, Systematic Literature Review Article.
INTRODUCTION
COVID-19 is an infectious viral disease that affects the respiratory system. To control rapidly spreading diseases and pandemics we use isolations or quarantines. Quarantine or isolation is defined as ‘Quarantine’ is defined as the restriction of movement, upon an individual or a group of people to restrain them at a designated facility or in their homes. It is basically separation of healthy people from those who may have been exposed to the pathogen. The whole concept is to keep a track of people who may develop symptoms and ensure early detection of disease. It is one of the oldest techniques to control pandemics and contagious diseases [1]. Its human to human transmission through air droplets meant people had to restrict themselves from social activities. The World Health Organization recommended social distancing and isolation as most effective ways to prevent its transmission in absence of a vaccine. Isolation is defined as Separation of sick people with a contagious disease from those who are not sick. Even though isolation measures are taken to protect humans, it takes a great toll on human mental health. The sudden Coronavirus pandemic enhanced social distancing and self-isolation that has affected all the facets of mental health, emotional health, and psychological and social wellness at the collective level [2]. On February 26, 2020, Pakistan reported its inaugural COVID-19 case, prompting an immediate outbreak declaration. During the COVID-19 pandemic in Pakistan, rates of depression stand at 33 % (72.9 million), anxiety at 40 % (88.4 million), PTSD at 34.9 % (77.1 million), and stress at 27 % (59.6 million). Ever since the outbreak of Coronavirus, it has caused panic all over the world, with most people struggling mentally and physically. Those who were COVID +, isolation was the only way of treatment. Every patient in isolation experienced different symptoms [3].
Significance of the study
The concept of isolation is still new to human beings and we still need to adapt to new behaviour and attitudes. Isolation and quarantine are key measures in outbreak management and disease control. They are, however, associated with negative patient experiences and outcomes, including an adverse impact on mental health and lower quality of care due to limited interaction with healthcare workers.
Aim of the study
Till date there are no published studies on COVID-19 patient experiences in isolation in Pakistan. The purpose of this qualitative study is to explore the experiences and perceptions of patients going/went through isolation during COVID-19 illness.
Hence there is an effective need for a study to cover experiences, feelings of Covid19 patients during isolation, so that we have proper knowledge of how patients responded to isolation and how they cope with psychological distress.
METHODOLOGY
A qualitative study including COVID-19 patients who experienced isolation in Peshawar was conducted from 1st February 2021 to 15th March, 2021. It included 20 males of mean age around 20-35. Audio/telephonic interviews were conducted based on a well-structured. Sample size is 20 male; Questionnaire comprising seven questions, a copy of which is attached below. Before recording interviews, participants were well informed and explained regarding procedure, consent from each participant was taken.
In this qualitative study, a non-probability purposive sampling approach was applied.
All recorded interviews were transcribed and common themes were first analysed by two researchers. Conventional content analysis is a research method for the subjective interpretation of the text data content through the systematic classification process of coding and identifying themes or patterns. This type of analysis contributes significantly to a deeper understanding of human perceptions and experiences.
Later on the data was analysed through NVivo 10.
All participants were informed about the details of the study. Participation in the study was voluntary, and Patient could withdraw from the study without any consequences.
Suggestions on hospital isolation
Hospital policies and ward facilities can affect patients' activities of daily living. The days of hospital isolation motivated this study's patients to propose ideas and insights for improving isolation and recovery time in the isolation ward. The only issue with living in the ward was the lack of facilities. For example, I could not find places to hang clothes. Therefore, almost all my activities were limited to the bed. (P8). It happened that the hospital policy was changing when I was in the ward. Nurses had different perceptions of the rules of taking items into the isolation ward. No clear instructions were provided. Every time we would get a different answer.
Comprehension and though after recovery from COVID-19 after isolation
The understanding after recovery. The patients said that contracting COVID-19 and enduring multiple days of hospital isolation had made them more aware of the preciousness of life and given them unique insights. They hoped that they could help with the continuous improvement of the public health system and provide feedback to society by sharing their experiences and feelings. Because of this unique experience, I feel that I should cherish my life. I exercise more often and maintain good health. By exercising, I can breathe more vigorously, which makes me feel alive. I chose to publicise my experience and accepted multiple media interviews. I would like to share my hospitalisation experience and feelings with the public to make some improvements.
OUR STUDY RESULTS
Participant's Lived perceptions and experiences about COVID-19 isolation were represented by 4 themes.
- Response to isolation
- Un social changes during isolation
- Fear of outcomes
- Keeping yourself busy in isolation
These participants responded with both positive and negative experiences in this study, which are important for planning of further outbreaks.
Theme1) Response to isolation: All patient's initial response to COVID-19 was isolation, most patients gave negative response to isolation, they feared isolation, since for most it was first experience and staying away from family and friends was not a good experience, while some said it gave them time to reflect on themselves and their shortcomings. One of the participants said "Initially it was shocking. One thinks he has got the disease until the test comes positive but with time my thought process changes from pessimistic to Optimistic.
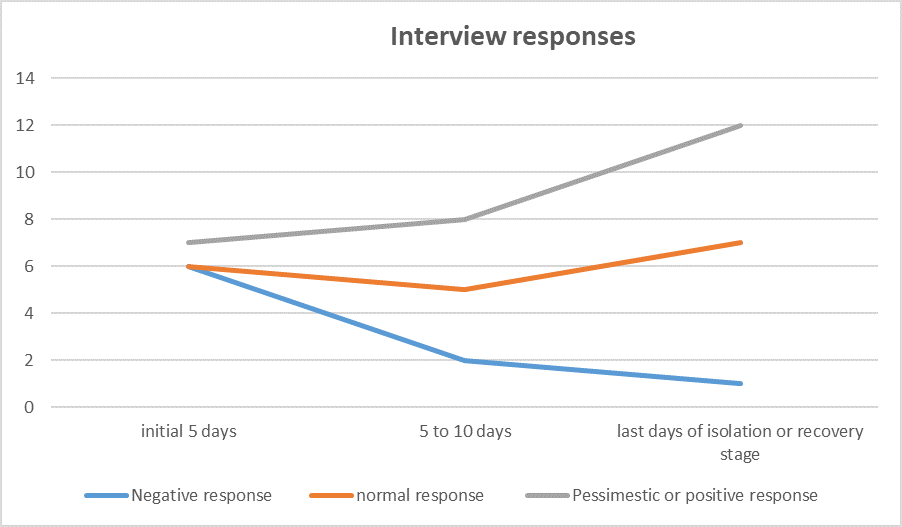
Table no.1:
Interviewer’s responses in terms of Negative, Normal and Pessimistic/Positive responses.
Different interview responses of covid patients in isolation: Initially; patient had very negative thoughts and slowly and gradually they got used to it and they got positive and pessimistic approaches.
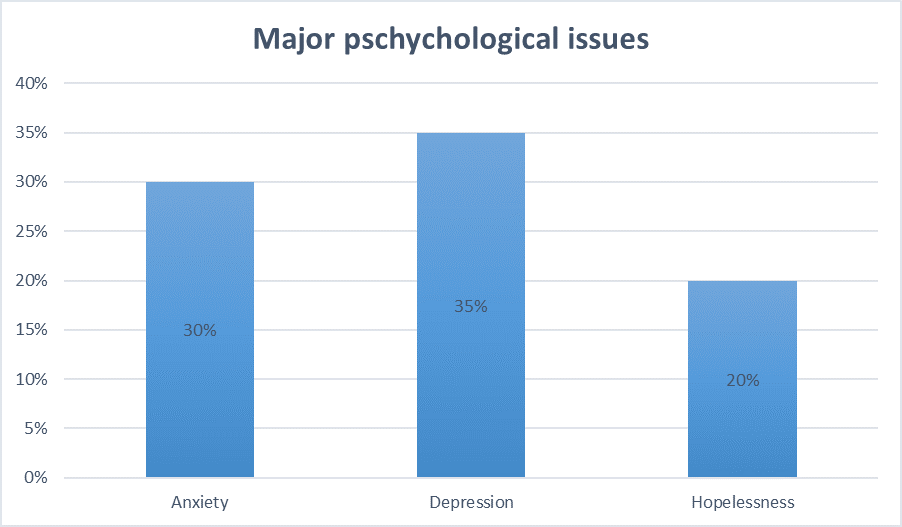
Theme2) Social changes during isolation: A number of patients complained of overthinking during isolation that led them to anxiety and depression and also staying away from family members made them feel lonely. One participant said” I didn't experience anything positive; it was all negative due to depression of being away from family. About 6/20 patients had anxiety and 7 /20 had depression and 5 patients had hopelessness.
Table no.2:
During covid isolation: patients had developed some sort of psychological issues, upon interviewing our patients we had taken anxiety, depression and hopelessness as our variables and we found that a major percentage of patients had these issues represented in the table.
Theme3) Fear of outcomes: most patients were worried about their family members that they might come in contact with virus and that lead patients to severe anxiety, another fear was progression to a more severe form of disease, all of this was making patient more fearful, most patients said they weren't stigmatised from virus, while some said It caused them stress and social stigma.
Theme4) keeping yourself busy in isolation: All patients agreed that keeping yourself busy during isolation was the best way to keep your mind healthy. They agreed on socially connecting with friends and keeping yourself busy can work during isolation.
Literature review on COVID-19 isolation patients:
Since Covid-19 is a new pandemic, review of literature doesn't properly describe the experiences and perceptions of patients during isolation and only information masses can get is from social media and this can spread a lot of misinformation among people and hence it would lead to psychological distress [4].
However, some Past studies suggest isolation has been linked to Post Traumatic Stress Disorder, anger and confusion. A qualitative study in Toronto during the SARS CoV-1 outbreak suggested that patients in isolation felt stigmatised, bored, blamed and rejected. A qualitative study in Australia covering lived experiences of COVID-19 patients in isolation reported negative experiences and unintended consequences of isolation including depression and aggression [5].
1-Health care quality:
A literature review on patient-centred care in the term of healthcare quality figures out how patient-centred care principles (like respect, emotional support, and clear communication) impact patients’ experiences, especially during pandemics like COVID-19.
2-impact of isolation on patient experience:
Studies that show isolation on patients' psychological well-being, including feelings of loneliness, anxiety, and depression. Isolation might amplify patients' needs for compassionate care and strong provider-patient communication [6].
3-Communication and Information Sharing:
Timely communication between healthcare providers and isolated patients for studies on communication methods (telemedicine, virtual visits, etc.) communication was used to support COVID-19 patients in isolation and their impact on patient satisfaction [7,8].
Quality of Mental Health Support during Isolation
Mental health services provided to isolated COVID-19 patients, particularly in inpatient and quarantine settings. Explore how quality mental health support affects patient experiences and overall perception of care [9].
Access to Resources and Support Systems
Explaining the role of healthcare quality in providing resources for isolated patients, such as access to medical updates, counselling, and social support services. Studies should focus on the disparities in resource allocation during COVID-19 and their impact on patient experiences [10-12].
Healthcare System Challenges and Innovations during COVID-19
Analyse how the healthcare system’s challenges during COVID-19 (e.g., resource shortages, overwhelmed staff) influence care quality for isolated patients. Include literature on innovative approaches, such as digital health solutions, and their effectiveness in maintaining care quality during patient isolation [13].
Patient Satisfaction and Perceived Quality of Care in Isolation
Examination of patient satisfaction and perceptions of healthcare quality during COVID-19 isolation. Look for factors that contributed to positive or negative perceptions, and how these may inform improvements in future pandemic response [14].
Impact on mental health: The social isolation and quarantine measures during the COVID-19 pandemic had a profound impact on mental health, contributing to increased levels of stress, anxiety, depression, and loneliness [15]. Prolonged separation from social support networks, disruptions to daily routines, and fear of illness created a heightened sense of uncertainty and emotional strain. For many, the lack of face-to-face interactions and the inability to engage in usual activities led to feelings of isolation, which exacerbated existing mental health conditions and triggered new psychological challenges. Vulnerable populations, including those with pre-existing mental health issues, were particularly affected, often experiencing a decline in their well-being due to the lack of coping mechanisms and external support [16].
Back to normal social and peaceful family and friend life: Returning to a normal social life and reconnecting with family and friends after the isolation of COVID-19 brought a renewed sense of joy and emotional relief for many. Reuniting with loved ones helped reduce feelings of loneliness and provided a support system to process the stress and anxieties experienced during quarantine. Sharing meals, engaging in group activities, and celebrating life’s milestones again rekindled a sense of normalcy and well-being. For many, these reconnections strengthened bonds, highlighting the importance of community and companionship in fostering resilience and mental health after a prolonged period of isolation [17].
DISCUSSION
There is very limited data which tells us about experiences of COVID-19 patients during isolation. This study focuses on fears and problems faced by patients during isolation and gives us an idea how we can overcome them and how we can prepare ourselves for future outbreaks like these. This study showed patients go through a wide range of emotions. During isolation including anxiety, fear, depression, anger [18]. This study revealed that hospital isolation during the COVID-19 epidemic affected patients physically, psychologically, socially, and spiritually. The majority of our study participants considered COVID-19 as preventable. Good Hygiene is considered to be one of the most effective preventive measures of communicable diseases. Handwashing is an important basic personal hygiene that can help in reducing transmission of COVID-19. Social and psychological impacts identified through this study centred around our key theme of ‘loss’ [19]. Practical social and economic losses—the loss of (in-person) social interaction, loss of income and loss of structure and routine—led to psychological and emotional losses—the loss of motivation, loss of meaning and loss of self-worth. The study's patients recollected their rich experiences of the negative emotions they had felt: fear (especially after the diagnosis), concern about transmitting the virus to relatives and friends, social isolation during the isolation, uncertainty about the disease progression during treatment, and disappointment when positive test results meant they could not yet leave the isolation ward [20]. Their fear, boredom, and social withdrawal increased as their stays in the isolation ward extended. Patients overthink a lot during isolation. We found that the isolated patients compromised owing to the highly contagious nature of the disease. Previous studies have shown that those who experienced isolation felt stigmatised, bored, blamed, and rejected. Our results confirmed that despite the stressful effects of hospital isolation, the interviewees tried to remain optimistic, actively tracked information about the pandemic, and improved their understanding of the pandemic and the disease itself [21]. Most participants felt worried about their family members and fear of developing a serious illness. An effective mechanism for taking care and treating fears of these patients should be made. This study gives us an idea that we should try to connect them more with health care workers and psychologists and try to change people's behaviour and make it more positive [22]. Also, we used video and telephone interviews, which can hamper observations of nonverbal behaviours, including body language and facial expressions, and make it more difficult to communicate with an interviewee. The use of electronic devices might also affect people's willingness to participate in long interviews and shorten interview times [23].
Loss of motivation, loss of meaning and loss of self-worth
Many participants felt that the social distancing and isolation have significant social and psychological impacts on their lives, central to which was a feeling of loss. Consisted of three practical, social and economic losses: loss of (in-person) social interaction, loss of income and loss of structure and routine. These in turn led to psychological and emotional losses.
Depression
A number talked about feeling depressed or anxious as a result of social distancing or isolation, an experience someone in a prison. Secondly, a number of participants show a loss of income, either permanent loss of a job, or through temporary loss (via lost clients or customers or being furloughed), had left them feeling ‘quite depressed’. Thirdly, a loss of structure and routine, which for some had left them feeling ‘less active’ or ‘sluggish’. Professional mental health support, less than 2 weeks into isolation. Participants also spoke of a loss of motivation to perform basic everyday tasks, such as personal hygiene and grooming or exercising, and how this demotivation was having an effect on their physical health. Sometimes feeling a loss of ‘self-worth’ [24].
Lack of trust in, and clarity of, government communication around social distancing and isolation
Many participants described a lack of trust either in government, who were seen to be politicising the pandemic. COVID-19 made them feel in both a physical and an emotional sense. Seeing others in a heightened state of anxiety makes it harder to suppress it in yourself. All participants reported being highly adherent to government instructions on social distancing. Participants also displayed a high degree of social consciousness, with many acknowledging that despite not perceiving themselves as being at high risk, they were doing it to save lives and protect those most vulnerable to the disease. Despite reporting their own high degree of adherence, many participants suggested that they had observed instances of non-adherence in others. First, non-adherence was seen to be due to a lack of social conscience. Second, non-adherence was seen to be due to a lack of understanding. Participants argued that people who were not observing social distancing lacked knowledge over how they could help spread the disease even if they themselves were not exhibiting symptoms [25].
CONCLUSION
Worldwide the pandemic had caused the social and personal lives of human beings to change drastically, the patients initially had negative responses and thoughts regarding isolation in the first week, once time passed, they got used to it and response changed from negative to positive responses in a short time. Psychologically about one third of patients had developed anxiety, depression and hopelessness. Patients had fear of progression of disease but slowly and gradually they got used to it and they developed certain ways of keeping themselves busy such as in tele education and socializing with friends on different social applications using the internet.
ACKNOWLEDGMENTS
None.
CONFLICTS OF INTEREST
There is no conflict of interest.
REFERENCES
- World Health Organization. (2020). Director General's opening remarks at the media briefing on Covid 19.
- Brooks, S, Woodland, L, Webster, R. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The lancet. 395(10227):912-920.
- Robertson E, Hershenfield K, Grace SL, Stewart DE. (2004). The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. Can J Psychiatry. 49(6):403-407.
- Shaban RZ, Nahidi S, Sotomayor-Castillo C, Li C, Gilroy N, O'Sullivan MVN, et al. (2020). SARS-CoV-2 infection and COVID-19: The lived experience and perceptions of patients in isolation and care in an Australian healthcare setting. Am J Infect Control. 48(12):1445-1450.
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J; China Novel Coronavirus Investigating and Research Team. (2020). A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 382(8):727-733.
- Hayat K, Rosenthal M, Xu S, Arshed M, Li P, Zhai P, et al. (2020). View of Pakistani residents toward coronavirus disease (COVID-19) during a rapid outbreak: a rapid online survey. Int J Environ Res Public Health. 17(10):3347.
- Heymann DL, Shindo N. (2020). COVID-19: what is next for public health? Lancet. 395(10224):542-545.
- Wilder-Smith A, Freedman D. (2020). Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 27(2):taaa020.
- Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. (2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 55:105924.
- Forni G, Mantovani A. (2021). COVID-19 vaccines: where we stand and challenges ahead. Cell Death Difer. 28(2):626-639.
- Guan W-j, Ni Z-y, Hu Y, Liang WH, Ou CQ, He JX, et al. (2020). Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382(18):1708-1720.
- Batra K, Urankar Y, Batra R, Gomes AF, Kaurani P. (2021). Knowledge, Protective Behaviors and Risk Perception of COVID-19 among Dental Students in India: A Cross-Sectional Analysis. In: Healthcare. Basel: Multidisciplinary Digital Publishing Institute.
- Mirza TM, Ali R, Khan HM. (2020). The knowledge and perception of COVID-19 and its preventive measures, in public of Pakistan. PAFMJ. 70(2):338-345.
- Zhong B-L, Luo W, Li H-M, Zhang Q-Q, Liu X-G, Li W-T, et al. (2020). Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 16(10):1745.
- Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. (2020). Study of knowledge, attitude, anxiety & perceived mental healthcare needs in Indian population during COVID-19 pandemic. Asian J Psychiatr. 51:102083.
- Nemati M, Ebrahimi B, Nemati F. (2020). Assessment of Iranian nurses’ knowledge and anxiety toward COVID-19 during the current outbreak in Iran. Arch Clin Infect Dis. 15(COVID-19):e102848.
- Karim A, Akter M, Mazid AT, Pulock OS, Aziz TT, Hayee S, et al. (2020). Knowledge and attitude towards COVID-19 in Bangladesh: population-level estimation and a comparison of data obtained by phone and online survey methods.
- Abdi M, Mirzaei R. (2020). Iran without mandatory quarantine and with social distancing strategy against coronavirus disease (COVID-19). Health Secur. 18(3):257-259.
- Webster RK, Brooks SK, Smith LE, Woodland L, Wessely S, Rubin GJ. (2020). How to improve adherence with quarantine: rapid review of the evidence. Public Health. 182:163-169.
- Prime Ministers’ Office. PM statement on coronavirus. Available: https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-12-march-2020 Google Scholar
- Imani JH. (2020). Social impacts of the spread of coronavirus in Iranian society. Soc. Impact Assess. 1(1):87-103.
- Kofman YB, Garfin DR. (2020). Home is not always a haven: The domestic violence crisis amid the COVID-19 pandemic. Psychol. Trauma. 12(S1):S199–S201.
- Donohue JM, Miller E. (2020). COVID-19 and school closures. JAMA. 324(9):845-847.
- Islam MA, Barna SD, Raihan H, Khan MNA, Hossain MT. (2020). Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PloS One. 15(8):e0238162.
- Lebow JL. (2020). The challenges of COVID‐19 for divorcing and post‐divorce families. Fam. Process. 59(3):967-973.