Previous Issues Volume 9, Issue 7 - 2024
Leveraging BioFire FilmArray (Multiplex Polymerase Chain Reaction) to Unmask Varicella Zoster Virus Meningoencephalitis: A Rare Case Report of Geriatric Neuro-Infection from North India
Arushi Gupta1,*, Balram JI Omar2, Panda PK3, Minakshi Singh4, Chetna Maharia5
1Junior Resident, Department of Medical Microbiology, AIIMS Rishikesh, India
2Professor, Department of Medical Microbiology, AIIMS Rishikesh, India
3Additional Professor, Department of Internal Medicine, AIIMS Rishikesh, India
4Senior Resident, Department of Medical Microbiology, AIIMS Rishikesh, India
5Junior Resident, Department of Diagnostic and Interventional Radiology, AIIMS Rishikesh, India
*Corresponding author: Arushi Gupta, Junior Resident, Department of Medical Microbiology, AIIMS Rishikesh, India, Tel: 9779268784, Email: [email protected]
Received Date: June 09, 2024
Published Date: July 31, 2024
Citation: Gupta A, et al. (2024). Leveraging BioFire FilmArray (Multiplex Polymerase Chain Reaction) to Unmask Varicella Zoster Virus Meningoencephalitis: A Rare Case Report of Geriatric Neuro-Infection from North India. Mathews J Case Rep. 9(7):177.
Copyrights: Gupta A, et al. (2024).
ABSTRACT
Meningoencephalitis typically presents with fever and signs of meningeal irritation thereby, making it difficult to distinguish bacterial, viral and fungal aetiology merely on clinical examination. Therefore, the use of multiplex PCR (Polymerase Chain Reaction) targeting multiple etiological agents enhances accurate diagnosis and shortens turn-around time. We hereby report a case of acute VZV (Varicella zoster virus) encephalitis with superadded bacterial infections in an elderly male patient diagnosed via Biofire FilmArray, in Uttarakhand region of North India.
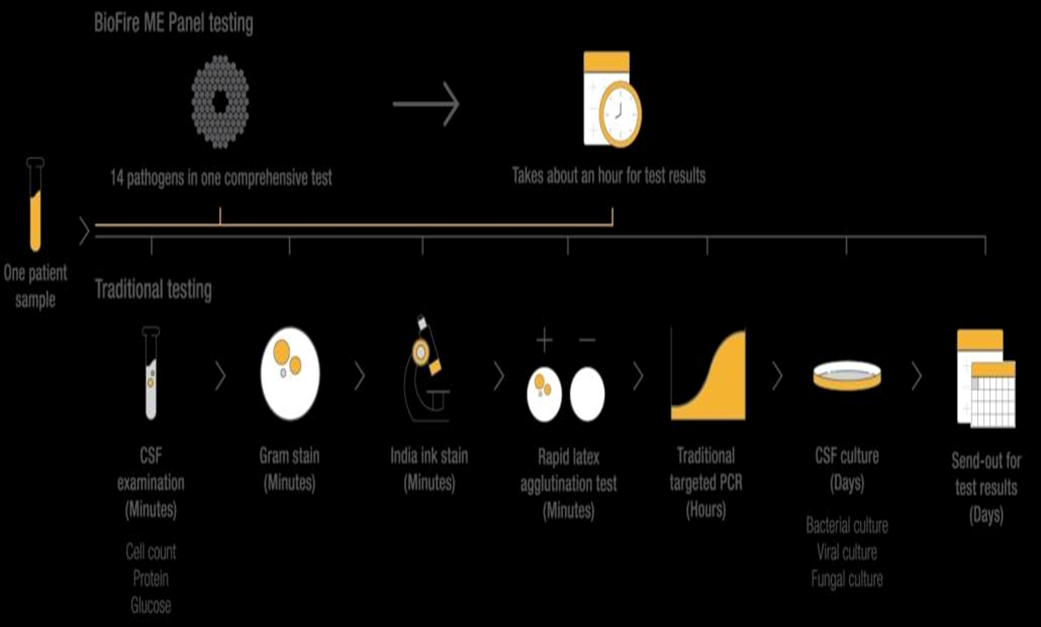
A 69-year-old male patient presented to Emergency department of AIIMS, Rishikesh with complaints of fever, headache, projectile vomiting and altered mental sensorium from where he was admitted in General Medicine HDU (high dependency unit) with a working diagnosis of acute meningoencephalitis. Film Array meningoencephalitis (ME) panel (BioFire Diagnostics, LLC, Salt Lake City, Utah) [1] combining 14 pathogens into a single cartridge-based nested multiplex PCR was performed as a point-of-care test. Various lab investigations including CSF counts, aerobic cultures, microscopy, CSF CBNAAT, MRI, NCCT Head, EEG were also done to rule out other potential causes.
Microscopic staining analysis and cerebrospinal fluid culture were both negative. However, CSF Biofire came positive for VZV guiding precise treatment. VP (Ventriculo Peritoneal) shunt was placed in view of obstructive hydrocephalus revealed on NCCT-head. Repeated interventions like intubation, co-morbidities and geriatric age group lead to development of VAP (Ventilator Associated Pneumonia) due to super added bacterial infection for which culture guided antimicrobial therapy was given. Full course of appropriate antiviral treatment was given, and patient was discharged in a haemodynamically stable condition.
Keywords: Geriatric Patient, Molecular Diagnosis, Neuro-infections, POCT (Point of Care Test), Syndromic Diagnosis, Viral Infections.
INTRODUCTION
Varicella zoster virus (VZV) is a virus of the alpha herpesvirus family that is neurotropic and has double-stranded DNA. The first exposure to this virus usually occurs in childhood, and the primary infection causes chickenpox, in which VZV becomes latent in the cranial nerve, spinal cord, and autonomic ganglia throughout the neuraxis [2].
Since the immune response to the virus is mainly mediated by T cells, reactivation usually occurs with aging or because of immunosuppression. Herpes zoster, also known as shingles, is caused by the reactivation of latent VZV in the dorsal root ganglion or trigeminal ganglion which manifests a bullous rash in the dermatomal distribution of sensory ganglia and acute neuritis [2].
VZV is one of the leading causes of infectious neurological diseases and the second leading cause of encephalitis and infectious meningitis. Mortality is 12-15%, which may be higher in immunocompromised patients. Therefore, swift diagnosis based on clinical manifestations, neurological symptoms, cerebrospinal fluid (CSF) analysis, and imaging abnormalities such as MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans is required to adequately manage and improve patient outcome. In addition, point of care tests (POCT) such as multiplex PCR play a vital role in accurate diagnosis.
Here we present a rare case of VZV meningo-encephalitis in a geriatric patient from a tertiary care center of Uttarakhand.
CASE SUMMARY
A 69-year-old male patient presented at the Emergency of AIIMS Rishikesh with altered mental status persisting for 4 days, accompanied by recurrent episodes of projectile vomiting and a single episode of fever 6 days prior. Initially treated at a district hospital in Kotdwar with conservative management. This undocumented pyretic episode was associated with chills and rigors with pulsatile holocranial headache which was relieved by antipyretics. The patient's deteriorating condition prompted referral to a higher-level facility. On arrival, the patient exhibited altered mental status (GCS - E3V4M6), blood pressure of 126/68 mmHg, a pulse rate of 98/min, respiratory rate of 22/min, and maintained Spo2 of 96% with 2 liters of oxygen support. Physical examination revealed neck rigidity and a positive Kernig sign. Additionally, the patient presented with abdominal lesions characterized by a central crust surrounded by redness, preceded by blister formation and associated with a burning sensation suggestive of a viral etiology. An urgent NCCT scan of the head and thorax (Refer to Table 3) revealed findings consistent with non-communicating hydrocephalus, right-sided pneumothorax, and mild mediastinal displacement.
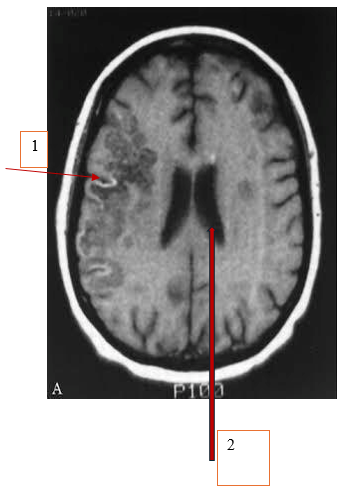
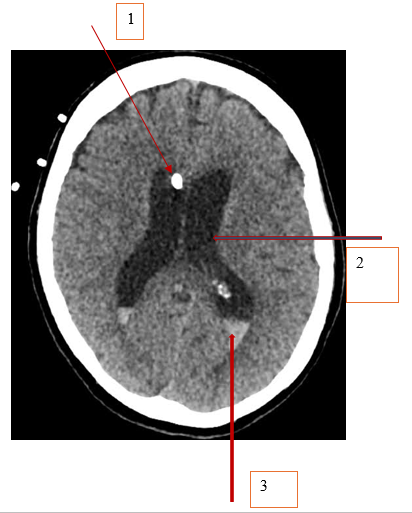
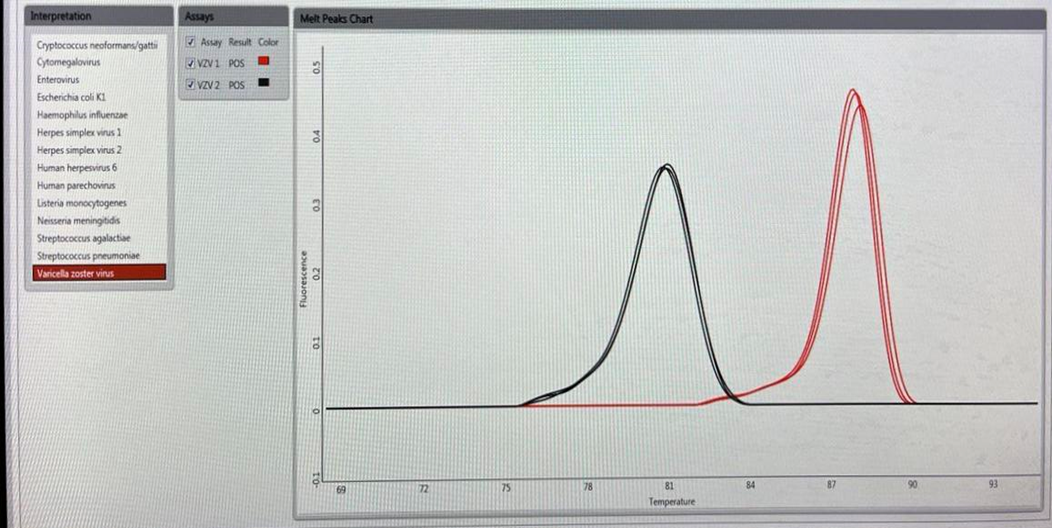
The patient was admitted to the High Dependency Unit and was initially managed for acute viral meningoencephalitis. On the third day of admission, a cerebrospinal fluid (CSF) examination was performed, and CSF Biofire [1] testing confirmed the presence of Varicella-Zoster Virus (VZV). The treatment regimen included Acyclovir, Meropenem, and Vancomycin. The patient who also had a history of hypertension and was on oral antihypertensive medications, experienced a sudden increase in blood pressure and a decline in sensorium on the fifth day of admission. Injectable anti-hypertensives were given to control blood pressure but due to persistent decline in sensorium, the patient was put on ventilatory support Consequently, he was transferred to the Medicine Intensive Care Unit for further management on the working diagnosis of acute viral meningoencephalitis with superadded bacterial infections. Neurosurgical consultation was sought, leading to the placement of an External Ventricular Drain (EVD) [Refer to Table 3] which resulted in an improvement in consciousness. Subsequently, due to a rise in blood counts and a decline in consciousness, the antiviral therapy was escalated to Ganciclovir. A repeat head CT scan) [ refer to table 3] revealed an enlargement of the hydrocephalus, necessitating the insertion of a Ventriculoperitoneal (VP) shunt by the neurosurgical team. Despite the procedure, there was no notable improvement in consciousness. An MRI of the brain as [described in Figure A] and was performed, revealing a significant intraparenchymal hemorrhage in the right frontal lobe, along with subarachnoid hemorrhage in the bilateral temporal and occipital lobes, as well as communicating hydrocephalus.
CBNAAT testing was conducted to rule out tubercular meningitis, yielding a negative result. However, due to strong suspicions of tubercular meningitis and ongoing low sensorium, empirical Anti-Tubercular Therapy (ATT) was initiated. Subsequently, the patient developed an iatrogenic pneumothorax, necessitating the insertion and subsequent removal of an Intercostal Drainage (ICD). A tracheostomy was performed to facilitate long-term ventilatory support, and ventilator-associated pneumonia caused by Klebsiella pneumoniae was treated with antibiotics guided by culture results. An EEG was performed to investigate Non-Convulsive Status Epilepticus (NCSE), revealing indications of diffuse cerebellar dysfunction. Biofire (1) confirmed the presence of Varicella-Zoster Virus (VZV), despite the patient's stable condition. Following a weaning trial, the patient was extubated and transferred to the High Dependency Unit (HDU), where ATT was discontinued. Due to the persistent positive VZV cultures, the patient was scheduled to receive Intravenous Immunoglobulins targeting VZV. The patient's overall condition notably improved in the subsequent days with appropriate management of bedsores and nutritional support through enteral feeding, leading to a discharge in a stable hemodynamic condition.
Figure A1. Sulcal hyperintensities seen along right cerebral hemispheres on T2 FLAIR MRI
Figure A2. Residual dilatation of supratentorial ventricles T2 FLAIR MRI
Figure B1. EVD in-situ on NCCT Head
Figure B2. Supratentorial hydrocephalus-dilatation of bilateral lateral ventricles on NCCT Head
Figure B3. Intra-ventricular haemorrhage in bilateral lateral ventricles on NCCT Head
Figure C. Biofire filmarray processing (1).
Figure D. BIOFIRE Melt curve peaks showing Varicella Zoster Virus positive.
Table 1. Hematological Investigations
|
INVESTIGATION |
20/11/2023 |
22/11/2023 |
24/11/2023 |
27/11/2023 |
13/12/2023 |
18/12/2023 |
21/12/2023 |
|
HB |
12.6 |
12.4 |
10.2 |
10.4 |
8.3 |
8.2 |
7.9 |
|
TLC (X1000) |
7.41 |
7.1 |
9.12 |
5.93 |
5.45 |
4.43 |
5.6 |
|
DLC(N/L) |
74.6/17.8/7.2/0.3/0.1 |
79.4/12.7/6.5/1.1/0.3 |
87/7/3 |
84/10/3 |
82/8/8 |
77/15/6 |
80/13/6 |
|
PLATELET |
99k |
108k |
98k |
112K |
133 K |
230K |
166K |
|
CSF |
15/11/2023 |
22/11/2023 |
|
TLC1 |
80 |
20 |
|
DLC2 |
M-70 / P- 30. |
M-65 / P- 35 |
|
SUGAR/PROTIEN |
86/256 |
88/260 |
|
CSF CULTURE |
STERILE |
STERILE |
|
CBNAAT3 |
NEGATIVE |
N/A |
|
ADA4 |
3.2 |
N/A |
TLC: Total Leucocyte Count; DLC: Diffrential Leucocyte Count; CBNAAT: Cartridge Based Nucleic Acid Amplification Test; ADA: Adenosine Deaminase
Table 3. Radiological Investigations
|
IMAGING |
FINDINGS |
IMPRESSION |
|
NCCT HEAD AND THORAX 13/11/23 |
THORAX
|
THORAX
|
|
IMAGING |
FINDINGS |
IMPRESSION |
|
NCCT HEAD 20/11/23 |
|
|
|
IMAGING |
FINDINGS |
IMPRESSION |
|
MRI BRAIN 28/11/23 |
|
|
DISCUSSION
Varicella-Zoster Virus (VZV) accounts for approximately 8-13% of all viral meningitis cases. While meningitis is a relatively uncommon manifestation of VZV, occurring in just 0.5% of infections, it remains a recognized complication [3]. Advanced age and immunocompromised states are thought to be key risk factors for the development of herpes zoster and other VZV reactivation symptoms [3] A dermatomal rash and neuritis are the most prevalent symptoms.
In this case, the patient presented with altered mental status for four days, along with recurrent vomiting and a previous episode of fever, indicating a potential diagnosis of acute meningoencephalitis. According to Lizzi J et al.'s study, VZV encephalitis typically presents with symptoms such as headache, fever, vomiting, altered consciousness, and convulsions. Additionally, focal neurological deficits like hemiparesis, cranial nerve paralysis, and abnormal osteotendinous reflexes may be observed [4]. However, our patient did not exhibit focal neurological signs. The most common symptoms of VZV encephalitis include a dermatomal rash [3] and neuritis, which align with our patient's presentation of characteristic lesions on the abdomen with a central crust, surrounding redness, vesicle formation, and a burning sensation, indicative of a VZV infection.
The adoption of BioFire Film Array meningitis/encephalitis as an initial point-of-care test has become widespread in various healthcare institutions due to its broad availability. In the case of the patient, the CSF BioFire [1] test yielded a positive result. This diagnostic panel screens for a range of pathogens, including Escherichia coli K1, Haemophilus influenzae, Listeria monocytogenes, Neisseria meningitidis, Streptococcus agalactiae, S. pneumoniae, CMV, enterovirus (EV), HSV-1, HSV-2, human herpesvirus-6 (HHV-6), human parechovirus (hPeV), VZV, Cryptococcus neoformans, and Cryptococcus gattii [1]. The advantage of this test lies in its ability to rapidly identify pathogens, enabling timely initiation of treatment, which is crucial in cases of central nervous system infections [5]. Early detection of VZV through BioFire testing allowed prompt initiation of antiviral therapy for the patient. The Infectious Diseases Society of America recommends intravenous acyclovir as the treatment of choice for VZV meningoencephalitis, with ganciclovir [6] considered an alternative agent [7]. In this case, the patient was initially treated with acyclovir and later transitioned to ganciclovir based on clinical evaluation.
Pathological studies indicate that VZV encephalitis is associated with vasculopathy in both large and small vessels [8]. MRI findings typically reveal ischemic or haemorrhagic infarctions in Gray and white matter, particularly at gray-white matter junctions, which are characteristic of VZV encephalitis. The MRI of the patient showed subacute haemorrhage involving the right frontal lobe, centrum semiovale, corona radiata, external capsule, basal ganglia region, extending to the right temporal lobe, with a mild small infarct in the left centrum semiovale.
Although the reason for the persistently positive VZV Biofire [1] could not be definitively determined, it led to the escalation of antiviral therapy and the consideration of Immunoglobulins against VZV. One plausible explanation could be polymicrobial sepsis in the patient, as evidenced by positive cultures for Pseudomonas aeruginosa, MR-Coagulase negative staphylococci, A. baumannii, Candida, and Klebsiella pneumoniae, further compromising the patient's immune status and potentially resulting in VZV shedding in CSF. The appropriate use of diagnostic tools like BioFire Film Array and targeted antiviral and antibiotic therapy contributed to the improvement of the patient's overall condition in this uncommon case of geriatric neuroinfection.
CONCLUSION
This case report underscores the significance of BioFire FilmArray in diagnosing Varicella-Zoster Virus (VZV) meningoencephalitis, a rare but potentially life-threatening condition, particularly in geriatric patients. The patient's presentation with altered mental status, vomiting, and fever, accompanied by characteristic VZV lesions, led to the suspicion of VZV infection. In addition to documenting an unusual presentation of positive Varicella zoster virus result on a meningitis/encephalitis panel, this case also emphasises the role of Biofire Filmarray as a Point of Care Test.
This multiplex PCR test confirmed the diagnosis, enabling prompt initiation of antiviral therapy. Imaging studies, including MRI and NCCT head, revealed characteristic features of VZV encephalitis, such as subacute haemorrhage and infarctions, as well as non-communicating obstructive hydrocephalus. EEG findings indicated generalized cerebral dysfunction. The patient's condition improved with targeted antiviral and antibiotic therapy, highlighting the importance of timely diagnosis and treatment in complex neuroinfections.
The unique ability of Biofire ensures identification of rare etiological agents which are difficult to diagnose conventionally. This case provides insights into how we can collaboratively enhance accuracy between various diagnostic modalities along with the use of clinical acumen, ultimately improving patient outcomes in cases of meningoencephalitis.
REFERENCES
- Syndromic Infectious Disease Diagnostics. BioFire Diagnostics. Available from: https://www.biofiredx.com/
- Sabbagh B, Seijari MN, Albuni MK, Barakat M, Alfitori GB. (2022). Varicella-Zoster meningitis with normal CSF cellularity: A rare case report. IDCases. 28:e01484.
- Nagel MA, Gilden D. (2013). Complications of varicella zoster virus reactivation. Curr Treat Options Neurol. 15(4):439-453.
- Lizzi J, Hill T, Jakubowski J. (2019). Varicella Zoster Virus Encephalitis. Clin Pract Cases Emerg Med. 3(4):380-382.
- Leber AL, Everhart K, Balada-Llasat JM, Cullison J, Daly J, Holt S, et al. (2016). Multicenter Evaluation of BioFire FilmArray Meningitis/Encephalitis Panel for Detection of Bacteria, Viruses, and Yeast in Cerebrospinal Fluid Specimens. J Clin Microbiol. 54(9):2251-2261.
- Collet A, Baes D, Mambie A, Hembert K, Boulle C, Gana I, et al. (2020). VZV meningoencephalitis treated with ganciclovir. Med Mal Infect. 50(5):444-445.
- Fellner A, White S, Rockwell E, Giandomenico D, Diaz MM, Weber DJ, et al. (2023). The clinical epidemiology, management, and outcomes of patients diagnosed with encephalitis in North Carolina, 2015-2020. J Clin Microbiol. 61(12):e0073123.
- Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. (2009). Varicella zoster virus vasculopathies: diverse clinical manifestations, laboratory features, pathogenesis, and treatment. Lancet Neurol. 8(8):731-740.