Previous Issues Volume 9, Issue 6 - 2024
Keloid Excision with Debulking Technique on the Left Ear Helix
Frien Refla Syarif, MD, Sp.DVE, FINSDV1,* Sri Lestari, MD, DR, Sp.DVE(K), FINSDV, FAADV2
1Ermedika Clinic, South Tangerang, Banten, Indonesia
2RSUP Dr. M.Djamil, Padang, West Sumatera, Indonesia
*Corresponding author: Frien Refla Syarif, MD, Sp.DVE, FINSDV, Ermedika Clinic, South Tangerang, Banten, Indonesia.
Received Date: June 10, 2024
Published Date: July 25, 2024
Citation: Syarif FR, et al. (2024). Keloid Excision with Debulking Technique on the Left Ear Helix. Mathews J Case Rep. 9(6):171.
Copyrights: Syarif FR, et al. © (2024).
ABSTRACT
Introduction: Keloids are benign dermal fibroproliferative lesions in connective tissue that usually appear in response to trauma and cannot heal spontaneously. The ear is one of the most common predilection areas for the growth of keloids and this condition can affect psychosocial patients to seek a doctor for cosmetic reasons or the presence of subjective symptoms of itching or pain. There are multiple treatment modalities of keloid, one of which is surgical excision with debulking technique. Case report: Reported one case of keloid on the left-ear-helix with complaints of a slight itchiness, measuring 5cmx2cm, as a result of a piercing that grew larger since 6 months after piercing. The case was treated by excision surgery with debulking technique using a local anesthetic injection Pehacain® (lidocaine2%+adrenaline1:80,000). At the end of wound closure, then one week after suture removal, and every 2weeks for 4times, 40mg triamcinolone-acetonide was given. The result of excision surgery was good and the patient was satisfied. Conclusion: Excision surgery with debulking technique was chosen because of the size of the lesion was quite large. Excision surgery with debulking technique on keloids was conducted to remove the keloid as fully as possible so that no keloid tissue remained at the predilection site. Administration of corticosteroids injection immediately after excision was done can reduce the proliferation of fibroblasts, synthesis of collagen and glycosaminoglycans and suppress pro-inflammatory mediators. to prevent keloid recurrence.
Keywords: Excision Surgery, Debulking Technique, Ear Keloid.
INTRODUCTION
Keloids are known as "confusing scars that are unknown to when they stop growing". These disorders include benign fribroproliferative lesions that grow as a response from an injury to the skin, inflammation, burns, or surgical incision. Keloids can also grow spontaneously without preceded by trauma. Keloids grow widely, are larger than the actual line of line and cannot heal spontaneously [1,2]. Keloids often form within the first year after an injury to the skin while persist and grow for years.
Several studies show an increase incidence of keloid in ear piercing activity of people over 11 years old [3]. Keloid rarely occurs on individuals aged over 65 years old [1]. People from African-American race appears to be suffering from keloid more often in comparison to Caucasian with a ratio of 5:1 and 16:1. Asians and Hispanics also have a high incidence of keloids, as too in identical twin individuals [2]. Contrastingly, keloid never occur in Albinos [1]. Keloids have a genetic predisposition with autosomal dominant patterns [6], but can also occur without a family history of keloids [1]. Familial keloids also found in two rare syndromes, Rubinstein-Taybi syndrome and Goeminne syndrome [4].
The pathological mechanism of keloids is an imbalance between the anabolic (proliferation) and catabolic (apoptotic) phases of wound repair [5]. Other hypotheses show that autoimmune sebum secreted intradermally triggers granuloma autoimmune responses.
Main criteria for selection of keloid management are those that have a low recurrence ratio, provide aesthetic improvement and significantly improve keloid condition, in addition to have minimal side effects [3]. Although there are many therapeutic modalities that can be chosen as keloid management, due to lack of level-one evidence, there is no single treatment to become the gold standard because of the high recurrence and the difficulty to discover keloid resolution ratios [2].
Prevention is a first-line therapy for keloids, including administration of antibiotics that are suitable for preventing infection, wound closure with normal tension, and if possible, incisions made should not cross joint spaces and excision is performed in line with skin tension lines [6]. In order to eliminate keloid lesions and prevent recurrence surgical treatment is necessary in combination with one or more other therapeutic modalities [5,6]. The most common procedure is surgery followed by corticosteroid injection [6]. Corticosteroids can reduce fibroblast proliferation, collagen synthesis and glycosaminoglycans, increase collagen degradation with a decrease in collagenase inhibitors and suppress collagen inhibitors proinflammatory mediator [7].
Amidst choices of keloids treatment in the ear, regardless of size, surgery is the gold standard because in addition to removing the mass it fixes the imperfect shape [3]. Corticosteroid injections performed immediately after the surgical operation of keloid excision show a decrease in transcription of collagen pro-alpha1 (I) associated with keloids. Intraoperative administration of triamcinolone acetoneid has also been shown to stop the growth of hypertrophy and keloid initiation rates [3,6].
Interrupted sutures are recommended for wound closure. For broad keloids, a flap or graft is performed which closes the wound without tension. The recommended thread to cover the wound for keloid surgery is nylon thread size 5.0 or 6.0 to avoid wound dehiscence. The sutures are opened after 10-20 days [1,6]. Injection of triamcinolone astonid 40mg/ml is carried out a week after lifting the sewing. This is done to avoid the occurrence of wound dehiscence if the injection is done less than a week after lifting the suture [6]. After that repeat the injection of steroids every 2-3 weeks for 4 times to prevent keloid recurrence. The maximum dose of triamcinolone acetonide is 40mg/ml per injection session is 5 ml [1,6].
CASE ILLUSTRATION
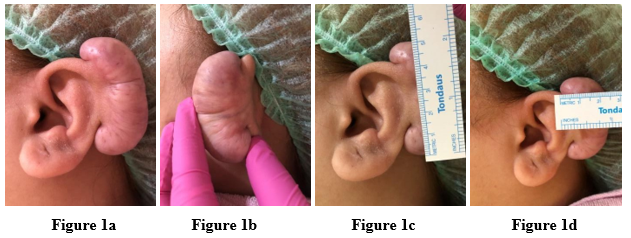
A female patient aged 21 years old has keloids in her left ear that have grown large since 6 months ago after piercing. They sometimes feel itchy and affect the patient's confidence therefore she wants the keloid removed. There is no previous history of treatment with keloids and there are no keloids on scars of other body parts. There is no history of family members who have widened scars from the actual wound limit with a slippery surface. The patient is physically examined to be within normal limits. Dermatological status found keloids measuring 5 cm x 2 cm on the left ear helix with a smooth, shiny, hard, mobile, and telangiectatic surface (figures 1a, 1b, 1c and 1d). Laboratory tests (blood clotting factors, blood sugar) is carried when HBsAg is normal. Informed consent has been signed by the patient.
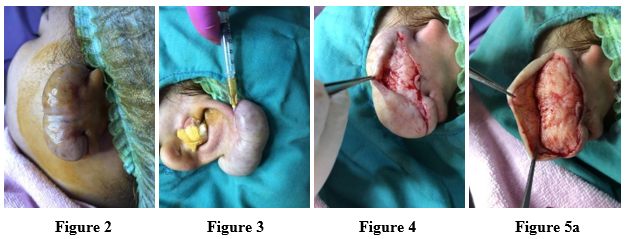
The patient undergoes surgical excision of the debulking technique as the following procedures are performed: (1) aseptic and antiseptic actions are performed with povidone iodine and alcohol 70% (figure 2); (2) local anesthetic is carried out at the base of the keloid using Pehacain® (lidocaine 2% + adrenaline 1:80,000) with a total injection of 2 ml (figure 3); (3) incision made from the posterior part of the keloid to open the skin (figure 4); (4) keloids are excised by debulking techniques and the remainder of the keloid is removed from the surrounding area (figures 5a, 5b, 5c); (5) an intra-keloidal debulking technique is carried out by sewing the remaining skin of the keloid tissue to cover the body using Prolene® size 5.0 (figure 6); (6) antibiotic ointment is applied and the wound is covered with a bandage.
The patient is given amoxicillin systemic antibiotic + clavulanic acid 625mg two times a day for five days and mefenamic acid analgesic 500mg three times a day with a recommendation to report ten days later. The postoperative area is recommended not to be exposed to water until the patient returns to remove the sewing. After 10 days, the wound has dried and the skin has completely recovered. Suture removal is then performed. A week after suture removal, the patient returns for injection of triamcinolone acetonide 40mg/ml for 1ml along the scar. In addition, the injection will be performed again thrice in intervals of 2 weeks. The post-operative results are good and the patient feels satisfied.
DISCUSSION
Keloid is a skin disorder that is difficult to manage because of the high recurrence rate. Although there are many theories about keloid growth, the exact etiology is still unknown. Osman, et al. states that an autoimmune response to sebum trapped in the dermis causes keloid growth [8]. Predilection, size and duration of keloids appearance in the ear affect the choice of therapy. Excision is performed on large keloids, by debulking technique, but recurrence rate in the selection of surgical excision therapy reaches fifty to a hundred percent [9]. Therefore, excision surgery is not used as a single therapy but is combined with adjuvant therapy such as corticosteroid injection, radiotherapy, pressure therapy and immunomodulatory [7].
In this patient surgical excision combination therapy with corticosteroid injection of triamcinolone acetonide 40mg/ml is selected to prevent keloid recurrence. Since the 1960s, intralesional steroid injection has been the most commonly used therapy for hypertrophic scars and keloids. Its main effects are suppressing the inflammatory process in wounds and suppressing the synthesis of collagen and glycosaminoglycans, inhibiting the growth of fibroblasts and increasing the degeneration of collagen and fibroblasts [7].
CONCLUSION
Excision surgery with debulking technique combined with intralesional injection of 40 mg/ml triamcinolone acetone is an option for the management of large size keloids in the ear. This technique can remove the keloid tissue as complete as possible and cover the body of the keloid with the rest of their tissue so that it can make the ear shape look ‘normal’ aesthetically and eliminate the symptoms caused by keloids. Additionally, also important is the ‘tension-free or minimal tension suture line’ done at the time of wound closure during keloid excision surgery. The exact time and distance of intralesional steroid injection are equally important so as not to cause wound dehiscence.
REFERENCES
- Kelly AP. (2009). Update on the management of keloids. Semin Cutan Med Surg. 28(2):71-76.
- Ud-Din S, Bayat A. (2013). Strategic management of keloid disease in ethnic skin: a structured approach supported by the emerging literature. Br J Dermatol. 169(Suppl 3):71-81.
- De Sousa RF, Chakravarty B, Sharma A, Parwaz MA, Malik A. (2014). Efficacy of triple therapy in auricular keloids. J Cutan Aesthet Surg. 7(2):98-102.
- Sobec R, Dobreanu C, Fodor L, Şomcutean A, Ţichil I, Cosgarea M. (2013). Ear keloids: a review and update of treatment options. Clujul Med. 86(4):313-317.
- Narakula GK, Shenoy RK. (2008). A prospective clinical review of "multi model" approach for treating ear keloids. Indian J Plast Surg. 41(1):2-7.
- Kelly AP. (2004). Medical and surgical therapies for keloids. Dermatol Ther. 17(2):212-218.
- Sharquie KE, Noaimi AA, Al-karhi MR. (2014). Debulking of keloid combined with intralesional injection of methotrexate and triamcinolone versus intralesional injection of methotrexate and triamcinolone. J Clin Dermatol Ther. 1:1-5.
- Kossi J, Peltonen J, Uotila P, Laato M. (2001). Differential effects of hexose and sucrose, and platelet derived growth factor isoforms or cyclooxygenase-1 dan 2 m RNA expression in keloid, hypertrophic scars and granulation tissue fibroblast. Arch Dermatol Res. 293:126-132.
- Nast A, Eming S, Fluhr J. (2012). German S2k guidelines for the therapy of pathological scars (hypertrophic scars and keloid). J Dtsch Dermatol Ges. 10(10):747-762.
.png)