Current Issue Volume 7, Issue 2 - 2024
Identification of Critical Risk Factors in CABG Surgery: A Survey-Based Expert Opinion Study
Ayşe Banu Birlik1,2,*, Hakan Tozan3, Kevser Banu Köse4, Yahya Yildiz5
1Graduate School of Engineering and Natural Sciences, Health System Engineering Program, Istanbul Medipol University, Istanbul, Turkey
2Department of Medical Services and Techniques, Istinye University, Istanbul, Turkey
3American University of the Middle East College of Engineering and Technology, Egaila, Kuwait
4Department of Biomedical Engineering, Istanbul Medipol University, Istanbul, Turkey
5Department of Anaesthesia and Reanimation, Medipol University School of Medicine, Istanbul, Turkey
*Corresponding Author: Ayşe Banu Birlik, Graduate School of Engineering and Natural Sciences, Health System Engineering Program, Istanbul Medipol University, Istanbul, Turkey & Department of Medical Services and Techniques, Istinye University, Istanbul, Turkey, Phone: +908502836000, ORCID: 0000-0001-5148-3784; E-mail: [email protected]
Received Date: November 12, 2024
Published Date: November 30, 2024
Citation: Birlik AB, et al. (2024). Identification of Critical Risk Factors in CABG Surgery: A Survey-Based Expert Opinion Study. Mathews J Surg. 7(2):34.
Copyrights: Birlik AB, et al. © (2024).
ABSTRACT
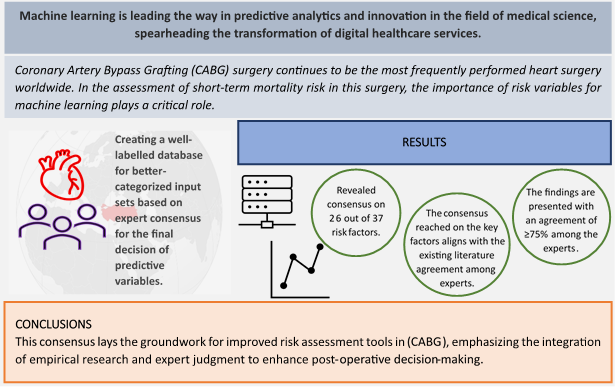
Introduction: Coronary Artery Bypass Grafting (CABG) surgery is a commonly performed cardiac procedure globally. This research represents the first step towards creating a machine learning-driven hybrid system for evaluating risks in CABG surgery. Therefore, the aim of this study is to identify reliable, unbiased, and prevalent risk assessment variables for the development of this system through a survey conducted among experts in the field of cardiovascular surgery. Methods: This research began with an extensive review of the literature, identifying 37 preoperative variables correlated with short-term mortality after CABG. A survey was sent to cardiovascular surgery experts, conducted via a secure Google Forms link, using a 5-point Likert scale to evaluate the importance of each factor. Consensus was defined as a factor receiving a rating of 4 or 5 from 75% or more of the participants. Results: The survey reached consensus on 26 out of the 37 identified risk factors. This analysis emphasised the experts' agreement on significant factors, consistent with prior studies on age, past vascular events, and conditions such as diabetes and renal dysfunction. The congruence between this study and the existing literature emphasised the significance of integrating both empirical data and expert opinions in CABG surgery. Conclusion: This study identified the key risk factors for short-term mortality in CABG surgery, based on expert consensus. The results provide a foundation for the development of a more precise risk assessment tool driven by machine learning. By emphasizing the integration of empirical research and expert opinion, this study offers valuable insights for post-operative care and decision-making in CABG surgeries.
Keywords: Cardiovascular Surgical Procedures, Expert Opinion, Heart Disease Risk Factors, Risk Assessment.
Graphical Abstract
INTRODUCTION
Importance of Preoperative Risk Factors in CABG Surgery
Despite the advanced treatment and preventive measures in place today, coronary artery disease (CAD) remains one of the most common causes of death. CABG is the most prevalent among cardiovascular surgical treatments, reflecting the profound impact of cardiovascular diseases on global health [1]. To provide the most effective care to patients scheduled for CABG, it is essential to thoroughly understand the factors influencing the short-term and long-term outcomes post-procedure. The optimization of preoperative characteristics has been the primary method of preventing adverse outcomes. Measures to prevent these outcomes traditionally rely on known factors. It is known that factors such as increasing age, previous vascular events, proteinuria, and diabetes increase mortality rates following a CABG operation [2]. Significant advancements have been made in cardiac surgery over the past decade. The intense research activities in this field underline the collective effort to optimize patient outcomes post-CABG. Literature reviews reveal numerous factors influencing CABG outcomes. However, not all of these factors are systematically evaluated in every patient undergoing CABG surgery, making their practical implementation incomplete. Therefore, a thorough examination of the most influential factors and the formulation of strategic action plans focusing on these factors are of critical importance [3]. Risk assessment systems are crucial in informing patients about cardiac surgery options, allowing for informed decisions. These systems, used throughout treatment, help predict patient health outcomes. Integrating risk assessments into clinical decision support systems is increasingly vital, particularly for coronary artery disease patients undergoing surgical revascularization. Such patient-specific assessments at the individual level and clinical prediction models for institutional analysis are growing, aiding quality improvement and supporting multi-institutional research [4].
Current Risk Assessment Systems for Cardiac Surgery and the Role of Electronic Health Records
The European System for Cardiac Operative Risk Evaluation (EuroSCORE), EuroSCORE II, and the Society of Thoracic Surgeons (STS) Risk Score are key tools in Europe and the USA for predicting mortality post-cardiac surgery [5]. EuroSCORE II, an improvement over its predecessor, and the STS score have shortcomings in accurately predicting mortality in high-risk patients [6]. These models do not provide long-term prognosis after surgery and lack data for specific clinical scenarios or extracurricular conditions [7]. Models for CABG procedures are continuously updated to improve their algorithms, offering more objective assessments of perioperative mortality risk than subjective clinical interpretations. However, their reliability may vary due to data sources and geographical relevance, and their complexity can limit practical use. These tools are vital for accurate pre-surgery mortality predictions, guiding clinical decisions, optimizing preoperative care, resource management, and quality control [8]. They play a key role in customizing care, choosing surgical methods, and discussing treatment plans, thereby affecting patient health and healthcare system efficiency [9].
Electronic Health Records (EHR) are increasingly vital for personalized medicine and are widely adopted in healthcare. They contribute to the complexity of medical decision-making, necessitating their integration into Clinical Decision Support Systems (CDSS). Traditional CDSSs, based on knowledge-based structures, emulate medical experts' thinking through algorithms and rely on established rules and guidelines [10]). However, real-world medical decisions often surpass the scope of these standardized rules, highlighting the limitations of knowledge-based systems in addressing specific or rare scenarios. The growing interest in using EHR data with advanced data mining and machine learning techniques aims to enhance decision-making processes [11]. This integration should be approached cautiously to avoid biases and statistical errors. An optimal approach for decision support is emerging, combining data analysis and clinical expertise. This might involve experts assigning weights to clinical variables, thereby marrying statistical analysis with clinical significance [12].
Importance of Risk Variables for Machine Learning
Recent advancements in artificial intelligence (AI) have resulted in precise prediction models using large clinical datasets, thanks to enhanced computational power, data storage evolutions, and extensive EHR clinical knowledge. The impact of AI is evident in areas such as radiology, pathology, cardiology, and surgery, revolutionizing the healthcare field [13]. These developments enable diverse applications, from clinical decision support to patient management, shaping medicine's future. Machine learning, a key AI and data science branch, uses algorithms to predict outcomes from historical data, with increasing medical applications in diagnosis and prognosis, highlighting this trend [14,15]. Outcome metrics are significantly impacted by various input variables, making it crucial to consider all relevant factors to enhance model performance [16]. At the same time, excluding variables that naturally influence outcomes is essential to avoid causality issues and maintain the model's external validity. Efficiently filtering out irrelevant variables improves computation, model efficiency, stability, and significance, thereby enhancing learning processes and accuracy [13]. Unlike traditional methods, like logistic regression, machine learning offers advantages in characterizing complex risk factor interactions. This is particularly predominant in past post-cardiac surgery risk prediction research [17]. Therefore, our study aimed to identify critical factors for short-term mortality risk assessment following CABG surgery using an expert opinion method.
The subsequent sections of the article are structured as follows: The second section will provide a theoretical foundation within the scope of the expert opinion method and present a theoretical background of relevant studies. The third section elaborates on the research methodology, detailing data sources used and data analysis processes. The fourth section delineates the results obtained from the expert opinions survey and the derived meanings and inferences. The fifth and concluding section discusses the research outcomes and potential directions for future work.
RELATED WORKS
Significant research using expert opinion methodology has been conducted in areas such as peripheral artery disease (PAD), cardiovascular health (CVH), carotid intervention, transfusion practices, and sleep medicine. These studies play a crucial role in enhancing clinician awareness, optimizing disease management, and improving patient outcomes. The expert opinion method, applied across specialties including vascular surgery, is a key tool in consensus-building among clinicians [18-20]. In particular Beamish et al. emphasize that expert opinions are a critical tool in consensus processes [18].
Neilson et al. sought to identify meaningful outcome measures for stakeholders regarding CHD drugs. Experts were surveyed on 16 CHD-related indicators, rating their importance on a five-point Likert scale and choosing the top three most meaningful outcomes. "Prevention of heart attack" was chosen as the most meaningful outcome (80%), followed by "prevention of death" (76%) [21]. The study's findings confirm the benefit of clinical CHD outcome measures used for value-based drug contracts. Singh et al. conducted a study using a modified Delphi process to identify and prioritize strategies for enhancing CVH care in resource-limited settings, aiming to guide research on multi-component strategies' effectiveness in low and middle-income countries [22]. Barrios et al. performed a literature review on PAD quality outcome indicators and utilized the Delphi technique to reach consensus on core indicators, resulting in twelve proposed quality indicators, including two composite parameters for major cardiovascular and extremity events [23]. Meershoek et al. highlights the absence of specific studies and defined European Society of Vascular Surgery guidelines for acute stroke management post-carotid interventions [24]. An international panel was convened to create a consensus-driven strategy and treatment decision tree for stroke during or after carotid endarterectomy in hospitals, focusing on understanding how perceptions of transfusion risks and safety impact transfusion decisions. In a study by Bourque et al., surveys were distributed to transfusion decision-makers in 33 Michigan cardiac surgery programs [25]. The study aimed to assess provider-reported transfusion trends in ten clinical scenarios using a six-point Likert Scale. It focused on how individual beliefs about transfusion risk and safety might influence transfusion tendencies, despite established scientific evidence and guidelines. Berezin et al. emphasize that sleep disorders, affecting up to 25% of the general population, increase the risk of adverse perioperative events [26]. The study aimed to identify the most critical sleep medicine topics in anesthetic practice. Expert opinions on sleep medicine topics that should be included in anesthesia specialization training were sought. Mei et al. emphasizes the lack of consensus on anal fistula recurrence (AFR) risk factors despite extensive research [27]. The authors aimed to provide an evidence-based overview of AFR risk factors from a global perspective, covering patient, surgery, and fistula aspects. These findings could aid in creating tools for early AFR detection in high-risk patients. Ultimately, consensus was achieved on 14 statements across three domains concerning AFR risk factors. Ferrer et al. conducted a systematic review and expert consensus study to identify risk factors (RFs) associated with infection progression in patients colonized with carbapenem-resistant Gram-negative bacteria (CRGNB) [28]. They identified 19 RFs associated with pneumonia development after respiratory colonization and 44 RFs related to infection progression after rectal colonization. Based on the consensus of experts, there are 13 RFs associated with the development of pneumonia after respiratory colonization with CRGNB, and 33 RFs associated with the progression of infection after rectal CRGNB colonization.
METHODOLOGY
Study Design
A comprehensive literature review was conducted to identify articles that elucidate factors influencing CABG outcomes. Tu et al. identified a set of six core variables (age, gender, sharpness, reoperation, left main coronary obstruction, and ejection fraction) that they believe provide the most important information for predicting outcomes of coronary artery bypass grafting (CABG), with little additional benefit from including additional variables [29]. Likewise, Jones et al. discerned seven principal determinants from the Cooperative CABG Database Project, which include age, gender, the acuity of left ventricular function, presence of left main disease, reoperation status, and the count of affected vessels [30]. In a study evaluating the predictive performance of a machine learning algorithm for operative mortality risk in cardiac surgery, Kilic et al. developed an XGBoost model that identified the most predictive individual risk factors to be latest serum creatinine, weight, age, height, ejection fraction, preoperative intra-aortic balloon pump, peripheral arterial disease, and diabetes mellitus [31]. Based on the STS National Cardiac Database, Shahian et al. found that the eight most significant predictors of mortality in cardiac surgery (age, surgical acuity, reoperation status, creatinine level, dialysis requirement, shock, chronic obstructive pulmonary disease, and ejection fraction) accounted for 78% of the variation in mortality explained by the full 28-variable model [32].
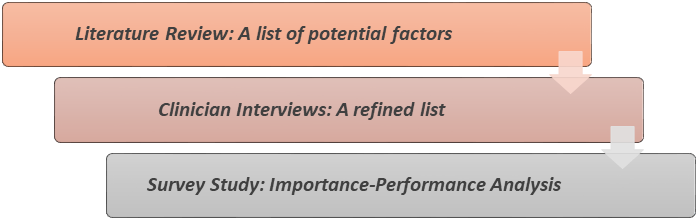
Figure 1. Flowchart Illustrating the Sequence of Events in the Expert Opinion Process.
The study followed a six-step design as shown in Figure 1. It involved selecting preoperative variables based on literature evidence and practicality. After consulting with Istanbul Medipol Mega University Hospital's information teams for data availability, the final variable selection was refined using clinician surveys and expert feedback. This approach ensures the development of a reliable, unbiased database for our risk assessment system.
Expert Opinion
Experienced professionals specializing in CABG outcomes participated in this consensus process. The experts were selected based on a rigorous set of criteria to ensure their relevance and expertise. The selection process included an initial invitation via email, which detailed the study's objectives and emphasized its voluntary and anonymous nature. The survey process was conducted between October and November 2023, allowing ample time for experts to provide their evaluations and feedback. Further details about the selection criteria for experts can be found in Section 3.4: Study Participants, which defines "cardiothoracic surgery specialists" as individuals meeting one or more of the following criteria. Experts were asked to evaluate preoperative risk factors using a five-point Likert scale, categorizing their importance as "Not at all important" to "Extremely important." Follow-up reminders were sent to increase participation. This study adhered to the ethical principles outlined in the 2008 Declaration of Helsinki. By ensuring a diverse and experienced group of participants, the research aimed to generate reliable and clinically significant insights into CABG risk factors.
Survey Administration
The survey was designed to collect expert opinions on risk factors that may impact short-term mortality following CABG surgery. Questions were formulated in categorical and ordinal measurements, as these types of measurements are easily comprehensible, can be collected online, and facilitate the integration of diverse expert perspectives. Categorical and ordinal measurements are less abstract compared to direct quantitative and probabilistic measurements. This allows us to leverage the concrete experiences of experts more effectively and minimize bias [33]. By focusing on the assessment of short-term mortality risk after CABG, a systematic literature review was conducted to identify factors influencing risk. Based on this literature review, we narrowed down the list of preoperative variables used in the study to the most crucial 37 parameters. Subsequently, we consulted clinicians regarding the scope and content of the list. Experts provided ratings and feedback (expert opinion) on the relative importance of the critical factors listed for the assessment of short-term mortality risk following cardiac surgery. Figure 2 illustrates the research process followed in this study.
Figure 2. Research Process Followed in This Study.
Experts in cardiothoracic and vascular surgery were initially contacted via email, providing details about the project and its voluntary, anonymous survey. Participants received a Google Forms link for a survey conducted in May 2023, where they rated the importance of risk factors affecting short-term mortality after CABG surgery on a five-point Likert scale, ranging from 1 (not important at all) to 5 (extremely important). This assessment utilized their knowledge, clinical experience, and available evidence. Clinicians assigned numerical weights to these factors based on their professional judgment for clinical decision-making. Two weeks after the initial email, follow-up reminders were sent, and 11 out of the 14 experts who had agreed to participate responded to the survey.
Study Participants
For the purpose of this study, we defined "cardiothoracic surgery specialists" as individuals meeting one or more of the following criteria: [20]
- Years of Professional Experience: Participants were required to have at least 5 years of active experience in cardiothoracic or vascular surgery, ensuring familiarity with CABG procedures and outcomes.
- Procedural Volume: Only those who performed or supervised at least 50 CABG surgeries annually were included. This threshold ensured substantial hands-on expertise and understanding of clinical complexities.
- Research Contributions: Experts with publications in peer-reviewed journals related to cardiac surgery or associated risk factors were prioritized to incorporate evidence-based insights into the consensus.
The participation of surgeons meeting the specified expertise criteria ensures that the insights gained in assessing short-term mortality risk after cardiac surgeries are more reliable and valuable.
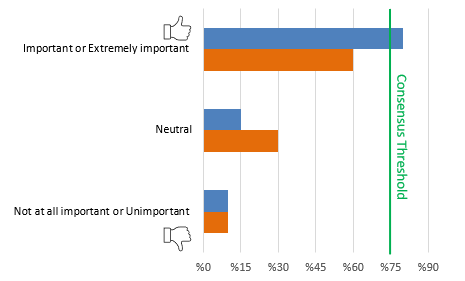
Consensus and Statistical Analyses
For each statement, consensus was determined through an assessment process based on the median Likert response and the interquartile range. Factors with a median value of 4 or 5 and a 25th percentile ≥4 were included in the final variable list. Consensus on the degree of importance of the risk factor, based on the literature, was defined as ≥75% agreement among experts (Likert scores of 4 and 5) or ≥75% of experts selecting it as the most significant indicator [21]. The criteria for determining the relevance of risk factors were as follows: [28]
- If a risk factor was rated as "5- Extremely important" or "4- Important" by ≥75% of the experts, these factors were considered relevant.
- If a risk factor had less than 75% agreement in any of the five scale items, the options "5- Extremely important" or "4- Important" were combined, and if it achieved ≥75% agreement, it was considered relevant.
- If additional information or explanations during the discussion session altered the interpretation of risk factors, the scoring could be re-evaluated and classified according to the criteria mentioned above.
- Experts may exclude risk factors that are difficult to assess or deemed uncertain from the scope of the study.
Descriptive statistics, including mean and standard deviation (SD), were employed to summarize the central tendency and variability of responses for each risk factor. Percentages were calculated for each response category to provide a detailed distribution of expert evaluations. To enhance the robustness of the consensus evaluation, a weighted average was applied, incorporating the SD to mitigate the impact of highly variable responses and ensure a balanced representation of expert opinions. Furthermore, risk factors with low agreement or those deemed ambiguous or difficult to assess were systematically excluded during expert discussion sessions, ensuring the relevance and clarity of the final list.
Table 1 provides a schematic representation of expert opinion. Data analysis was performed using Python programming with Pycharm IDE version 2022.3.1 (JetBrains individual licenses). The results of the evaluation of risk factors were collected in a database and presented as the percentage of responses given by experts to each option.
Table 1. Schematic representation of expert opinion
RESULTS
Establishing an Initial Set of Candidate Risk Factors
Based on a comprehensive review of the existing literature on risk factors associated with postoperative CABG, the research team identified a total of 37 distinct potential risk factors at varying levels of evidence and established this initial set.
Expert Opinion Survey Process Outcomes
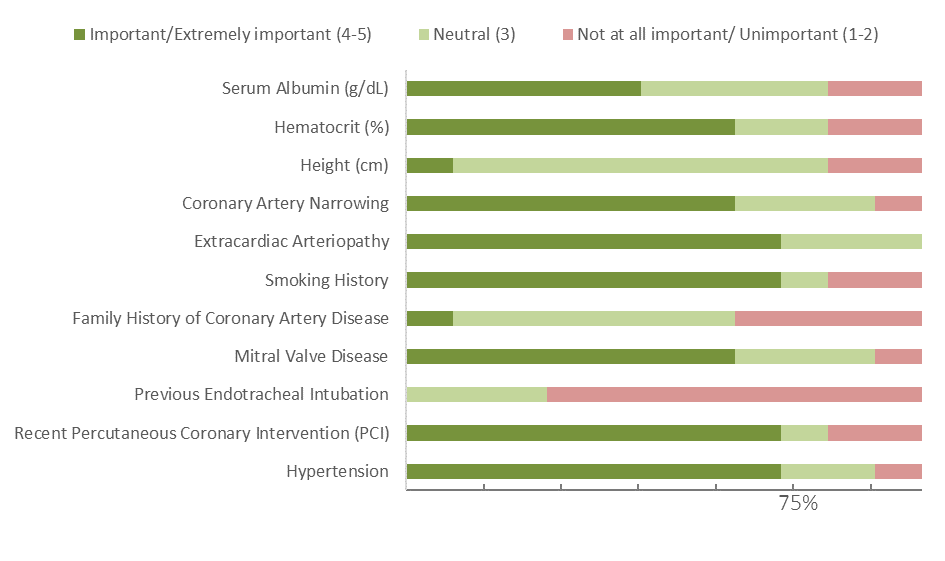
In the study, a focused and systematic consensus-building approach was utilized to identify key risk factors for short-term mortality following CABG surgery. This approach involved the participation of ten experts in the field, who provided comprehensive responses. The survey results, as summarized in Table 2 of the article, indicated that consensus was reached on 26 out of 37 risk factors, representing a consensus rate of over 75%. The method of analysis employed descriptive statistical techniques, presenting the percentages of participants who rated each risk factor across a spectrum of importance, ranging from "Not at all important/Unimportant [1-2]" to "Important/Extremely important [4-5]". Additionally, an average consensus score and a median value (25th percentile) were calculated for each risk factor to accurately represent the distribution and level of agreement among the experts.
A weighted average, considering the standard deviation (SD), was used to enhance the robustness of the expert agreement analysis. This detailed consensus process underscores the value of combining clinical expertise with evidence-based research. The agreement on risk factors, including age, past vascular events, and comorbidities like diabetes and hypertension, aligns with existing literature on their impact on post-CABG mortality rates [15,19]. The methodology and outcomes of this survey underscore the value of expert opinion in augmenting and refining risk assessment models, particularly in complex clinical scenarios like CABG surgery.
Table 2. Results of the expert opinion survey study. Consensus criteria were achieved, and these factors were found to be relevant
TIA: Transient Ischemic Attack; COPD: History of Chronic Obstructive Pulmonary Disease; Cardiogenic Shock, CPR: Cardiopulmonary Resuscitation; MI: Myocardial Infarction < (90 days); VSD: Ventricular Septal Defect; LVEF: Left Ventricular Ejection Fraction; Use of Mechanical Circulatory Support Device, Use of Inotropic Agents to Support Heart Contractility.
Table 2 illustrates the evaluation of preoperative risk factors in CABG surgery by experts. Factors were classified based on their perceived importance: ratings of 1-2 were considered "unimportant", 3 as "neutral", and 4-5 as "important" or "extremely important". For instance, factors such as diabetes mellitus, hypertension, and peripheral vascular disease were unanimously rated 4 or 5 by all experts, with high median scores ranging from 4.64 to 4.91. This indicates their crucial role in risk assessment for CABG surgery. The table's median and 25th percentile values clarify the experts' consensus and the factors' acceptability. Factors with a median score of 4 or 5 are widely acknowledged, suggesting they are pivotal variables in CABG risk analysis. These findings provide valuable guidance for refining and optimizing risk stratification processes before CABG surgery. According to the criteria outlined in Section 3.5, Consensus and Statistical Analyses, factors rated as '4- Important' or '5- Extremely Important' by less than 75% of the experts were not considered relevant (Table 3).
Table 3. Evaluation results of 'not relevant' risk factors
DISCUSSION
Our investigation has demonstrated notable congruence with the outcomes of preceding studies, such as those denoted as references [21-23]. These prior studies, which similarly employed expert opinion and the Delphi method across diverse medical domains, have established a foundation upon which our research builds. The concurrence of our study, particularly regarding the significance of diabetes mellitus, hypertension, and stroke, mirrors the emphasis placed on these conditions in preceding research. This alignment reaffirms the criticality of these factors in the context of CABG surgery risk assessment. Additionally, our results regarding the impact of peripheral vascular disease and liver disease as risk markers align with the findings of Barrios V. et al., and are supported by the consensus in the literature [23]. These studies, having underscored the pertinence of peripheral artery disease as a quality indicator, resonate with our findings. Additionally, our identification of preoperative states and renal dysfunction as principal risk factors aligns with the current literature's focus on patient-specific evaluations, highlighting the necessity of tailoring risk assessment to individual patient profiles. Nonetheless, our study is not without its limitations. The potential for response bias and the limitations inherent to a single-round consensus process must be acknowledged. These constraints reflect the challenges outlined in the studies by Meershoek et al. and Bourque et al., where the complexity of clinical situations and the variability in expert opinions hindered the achievement of a unified consensus [24,25].
This study has limitations typical of survey research, including potential response bias resulting from incomplete sampling and survey design. Factors such as hospital size, patient volume, and surgeon expertise are crucial because they influence expert perspectives, thereby affecting the generalizability of survey results. Conducted in a single round, the research's depth is limited. To improve outcomes, involving a diverse expert panel and multiple survey rounds is advised for greater scope and reliability. Our study aligns with existing literature on CABG surgeries, advocating for integrating empirical data with expert insights. This interdisciplinary approach is vital for enhancing patient care and decision-making, and it lays the groundwork for future development of advanced machine learning-based risk assessment tools, marking a significant step in evolving patient-specific medical strategies. Addressing the rising impact of CVDs requires focused efforts to fill knowledge gaps in innovative interventions. Expert opinions were used to identify risk factors for short-term mortality post-CABG. Understanding the economic implications of health financing structures and investments in quality enhancement is also crucial for policymakers [22].
CONCLUSIONS
This study identified key risk factors for short-term mortality following CABG surgery, emphasizing the importance of integrating expert insights with empirical evidence. While limitations such as response bias and the single-round survey approach may affect the findings, they highlight the need for further research involving more diverse expert panels and multiple survey rounds to enhance generalizability and reliability. The study serves as a foundation for developing a machine learning-based hybrid system for risk assessment in CABG. By selecting clinically and statistically significant variables, this approach bridges clinical expertise with advanced technology, paving the way for more precise and personalized risk stratification. Future work will focus on refining the algorithm and expanding its applicability to optimize patient care and decision-making in CABG surgeries.
FUNDING SOURCES
This research project, titled "Machine Learning-Based Risk Prediction System for Coronary Artery Bypass Surgeries," has been deemed eligible for support under The Scientific and Technological Research Council of Türkiye (TÜBİTAK) 1002-A Short term Support Module. This study represents the initial phase in achieving the project's objectives, marking a pivotal step towards the advancement of this research initiative.
DECLARATION OF COMPETING INTEREST
All authors have none to declare.
REFERENCES
- Feng X, Zhang C, Huang X, Liu J, Jiang L, Xu L, et al. (2023). Machine learning improves mortality prediction in three-vessel disease. Atherosclerosis. 367:1-7.
- Kusu-Orkar TE, Kermali M, Oguamanam N, Bithas C, Harky A. (2020). Coronary artery bypass grafting: Factors affecting outcomes. J Card Surg. 35(12):3503-3511.
- Bakaeen FG, Gaudino M, Whitman G, Doenst T, Ruel M, Taggart DP, et al. (2021). The American Association for Thoracic Surgery Expert Consensus Document: Coronary artery bypass grafting in patients with ischemic cardiomyopathy and heart failure. J Thorac Cardiovasc Surg. 162(3):829-850.e1.
- Coyan GN, Chin H, Shah A, Miguelino AM, Wang Y, Kilic A, et al. (2022). Charlson Comorbidity Index is Associated With Longer-Term Mortality and Re-Admissions Following Coronary Artery Bypass Grafting. J Surg Res. 275:300-307.
- Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, et al. (2009). The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg. 88(1 Suppl):S2-S22.
- Chalmers J, Pullan M, Fabri B, McShane J, Shaw M, Mediratta N, et al. (2013). Validation of EuroSCORE II in a modern cohort of patients undergoing cardiac surgery. Eur J Cardio-thoracic Surg. 43(4):688-694.
- Lee S, Jang EJ, Jo J, Park D, Ryu HG. (2022). Institutional case volume-incorporated mortality risk prediction model for cardiac surgery. Asian J Surg. 45(1):189-196.
- Campbell D, Boyle L, Soakell-Ho M, Hider P, Wilson L, Koea J, et al. (2019). National risk prediction model for perioperative mortality in non-cardiac surgery. Br J Surg. 106(11):1549-1557.
- Cromhout PF, Berg SK, Moons P, Damgaard S, Nashef S, Thygesen LC. (2019). Updating EuroSCORE by including emotional, behavioural, social and functional factors to the risk assessment of patients undergoing cardiac surgery: A study protocol. BMJ Open. 9(7):e026745.
- Antoniadi AM, Du Y, Guendouz Y, Wei L, Mazo C, Becker BA, et al. (2021). Current challenges and future opportunities for XAI in machine learning-based clinical decision support systems: A systematic review. Appl Sci. 11(11):1-23.
- Wang L, Chen X, Zhang L, Li L, Huang Y, Sun Y, et al. (2023). Artificial intelligence in clinical decision support systems for oncology. Int J Med Sci. 20(1):79-86.
- Pittams AP, Iddawela S, Zaidi S, Tyson N. (2022). Scoring Systems for Risk Stratification in Patients Undergoing Cardiac Surgery. J Cardiothorac Vasc Anesth. 36(4):1148-1156.
- Yoon HK, Yang HL, Jung CW, Lee HC. (2022). Artificial intelligence in perioperative medicine: a narrative review. Korean J Anesthesiol. 75(3):202-215.
- Arafat AA, Alamro S, Alrasheed MM, Adam AI, Ismail H, Pragliola C, et al. (2023). Applying machine learning methods to predict operative mortality after tricuspid valve surgery. Cardiothorac Surg. 31(16).
- Zhou N, Ji Z, Li F, Qiao B, Lin R, Jiang W, et al. (2022). Machine Learning-Based Personalized Risk Prediction Model for Mortality of Patients Undergoing Mitral Valve Surgery: The PRIME Score. Front Cardiovasc Med. 9(April):1-9.
- Weiss AJ, Yadaw AS, Meretzky DL, Levin MA, Adams DH, Mccardle K, et al. (2023). Machine learning using institution-specific multi-modal electronic health records improves mortality risk prediction for cardiac surgery patients. JTCVS Open. 14:214-251.
- Zhang N, Fan K, Ji H, Ma X, Wu J, Huang Y, et al. (2023). Identification of risk factors for infection after mitral valve surgery through machine learning approaches. Front Cardiovasc Med. 10:1050698.
- Beamish AJ, Johnston MJ, Harries RL, Mohan H, Fitzgerald JEF, Humm G, et al. (2020). Use of the eLogbook in surgical training in the United Kingdom: A nationwide survey and consensus recommendations from the Association of Surgeons in Training. Int J Surg. 84:199-206.
- Cornwell LD, Chu D, Misselbeck T, Lemaire SA, Huh J, Sansgiry S, et al. (2012). Predicting Mortality in High-Risk Coronary Artery Bypass : Surgeon Versus Risk Model 1. J Surg Res. 174(2):185-191.
- Sousa-Uva M, Head SJ, Thielmann M, Cardillo G, Benedetto U, Czerny M, et al. (2015). Methodology manual for European Association for Cardio-Thoracic Surgery (EACTS) clinical guidelines. Eur J Cardio-thoracic Surg. 48(6):809-816.
- Neilson LM, Swart ECS, Good CB, Shrank WH, Henderson R, Manolis C, et al. (2019). Identifying Outcome Measures for Coronary Artery Disease Value-Based Contracting Using the Delphi Method. Cardiol Ther. 8(1):135-143.
- Singh K, Joshi A, Venkateshmurthy NS, Rahul R, Huffman MD, Tandon N, et al. (2023). A Delphi Study to Prioritize Evidence-Based Strategies for Cardiovascular Disease Care in India. Glob Implement Res Appl [Internet]. 3(3):272-283.
- Barrios V, Beato P, Brotons C, Campuzano R, Merino-Torres JF, Mostaza JM, et al. (2022). Comprehensive management of risk factors in peripheral vascular disease. Expert consensus. Rev Clin Esp (Barc). 222(2):82-90.
- Meershoek AJA, de Waard DD, Trappenburg J, Zeebregts CJ, Bulbulia R, Kappelle JLJ, et al. (2021). Clinical Response to Procedural Stroke Following Carotid Endarterectomy: A Delphi Consensus Study. Eur J Vasc Endovasc Surg. 62(3):350-357.
- Bourque JL, Strobel RJ, Loh J, Zahuranec DB, Paone G, Kramer RS, et al. (2021). Risk and Safety Perceptions Contribute to Transfusion Decisions in Coronary Artery Bypass Grafting. J Extra Corpor Technol. 53(4):270-278.
- Berezin L, Nagappa M, Wong J, Clivatti J, Overdyk FJ, Margarson M, et al. (2021). Identification of Sleep Medicine and Anesthesia Core Topics for Anesthesia Residency: A Modified Delphi Technique Survey. Anesth Analg. 132(5):1223-1230.
- Mei Z, Li Y, Wang Q, Shao Z, Du P, Zhu J, Yang W, Ge M, Wang H. (2021). Risk factors for postoperative recurrence of anal fistula identified by an international, evidence-based Delphi consultation survey of surgical specialists. Int J Surg. 92:106038.
- Ferrer R, Soriano A, Cantón R, Del Pozo JL, García-Vidal C, Garnacho-Montero J, et al. (2022). A systematic literature review and expert consensus on risk factors associated to infection progression in adult patients with respiratory tract or rectal colonisation by carbapenem-resistant Gram-negative bacteria. Rev Esp Quimioter. 35(5):455-467.
- Tu J V., Weinstein MC, McNeil BJ, Naylor CD. (1998). Predicting mortality after coronary artery bypass surgery: What do artificial neural networks learn? Med Decis Mak. 18(2):229-235.
- Jones RH, Hannan EL, Hammermeister KE, Delong ER, O'Connor GT, Luepker RV, et al. (1996). Identification of preoperative variables needed for risk adjustment of short-term mortality after coronary artery bypass graft surgery. The Working Group Panel on the Cooperative CABG Database Project. J Am Coll Cardiol. 28(6):1478-1487.
- Kilic A, Goyal A, Miller JK, Gjekmarkaj E, Tam WL, Gleason TG, et al. (2020). Predictive Utility of a Machine Learning Algorithm in Estimating Mortality Risk in Cardiac Surgery. Ann Thorac Surg. 109(6):1811-1819.
- Shahian DM, Blackstone EH, Edwards FH, Grover FL, Grunkemeier GL, Naftel DC, et al. (2004). Cardiac surgery risk models: A position article. Ann Thorac Surg. 78(5):1868-1877.
- Brandt LA, Benscoter AM, Harvey R, Speroterra C, Bucklin D, Romañach SS, et al. (2017). Comparison of climate envelope models developed using expert-selected variables versus statistical selection. Ecol Modell. 345:10-20.
.png)
.png)