Previous Issues Volume 4, Issue 1 - 2019
Cytomegalovirus Retinitis in a 4-Year-Old Child with Acute Lymphoblastic Leukemia: Treatment and Prognosis
Jiancang Wang*, Feifan Du, Ming Su, Xiting Guo, Haixia Tian, Yanxia Song, Liya shang, Wei Zheng, Xiaoge Yang
Department of Ophthalmology, Hebei Children’s Hospital, Hebei Medical University, Shijiazhuang 050031, China.
Corresponding Author: Jiancang Wang, Department of Ophthalmology, Hebei Children’s Hospital, Hebei Medical University, Shijiazhuang 050031, China.
Received Date: Mar 12, 2019 Published Date: May 17, 2019
Citation: Wang J. (2019). Cytomegalovirus Retinitis in a 4-Year-Old Child with Acute Lymphoblastic Leukemia: Treatment and Prognosis. Mathews J Cancer Sci. 4(1): 17.
ABSTRACT:
Purpose: Children with acute lymphoblastic leukemia (ALL) are complicated with cytomegalovirus (CMV) retinitis due to the compromised immune function after chemotherapy. Here, we report a case of cytomegalovirus retinitis in a 4-year-old girl with ALL to emphasize the importance of early diagnosis and intravenous administration of antiviral medication in this group of patients.
Case Report: A 4-year-old girl with ALL was diagnosed of fulminant CMV retinitis after chemotherapy. Funduscopic examination revealed perivascular sheathing in pole and peripheral retina of right eye. Large areas of yellowish-white edema, hemorrhage and exudation along the vessels were seen in the superior nasal retina. Few perivascular sheathings were found in peripheral retina without obvious hemorrhage and exudation in left eye. With early diagnosis and prompt Intravenous administration of ganciclovir,the lesion of the fundus subsided and the vision was restored over 4 months of follow-up period.
Conclusions: In summary, CMV retinitis can occur in ALL pediatric patients who receive chemotherapy only, especially in the maintenance stage. With routine follow-up, early diagnosis and intravenous antiviral therapy, these patients may have a good prognosis.
Keywords: Cytomegalovirus Retinitis; Acute Lymphoblastic Leukemia; Early Diagnosis; Intravenous Antiviral Therapy
INTRODUCTION
H Cytomegalovirus (CMV), a ubiquitous herpesvirus, can cause severe disease with high morbidity and mortality in immunocompromised patients [1]. CMV retinitis is a serious viral eye infection of the retina, commonly in the form of necrotizing retinitis, which can potentially lead to blindness. CMV infection is commonly present in patients with advanced acquired immunodeficiency syndrome (AIDS), patients with immunodeficiency due to other etiologies are highly vulnerable to CMV infection.[2] CM retinitis has been described in ALL patients who received chemotherapy. However, only two cases of CMV retinitis have been reported in ALL children on chemotherapy [3, 4]. Herein, we reported a fulminant CMV retinitis in a 4-year-old girl with ALL on chemotherapy, with an emphasis on early diagnosis and prompt intravenous administration of antiviral medication.
CASE REPORT
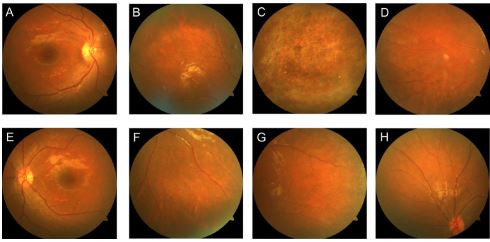
A 4-year-old girl, who presented with pale complexion and joint pain in 05/2015,was diagnosed as intermediate risk acute lymphoblastic leukemia in the Department of Hematology, Hebei Children’s Hospital.. Subsequently, she received systemic Chemotherapy, CCLG2008. After a week of the upper respiratory tract infection combined with later-onset pneumonia, she was referred to our department for diminution of vision. At initial examination, her best corrected visual acuity was 20/100 in the right eye (OD) and 20/40 in the left eye (OS). Slit-lamp biomicroscopic examination of the anterior chamber of the eyes was within normal limits. However, dust-like opacities in vitreous was discovered, especially in the right eye. Funduscopic examination revealed perivascular sheathing in pole and peripheral retina of right eye. Large areas of yellowishwhite edema, hemorrhage and exudation along the vessels were observed in the superior nasal retina (Figure1. A-D).
Figure 1: Fundus appearance at first visit (A-D: right eye, E-H, left eye): perivascular sheathing in pole and peripheral retina of right eye, large areas of yellowish-white edema, hemorrhage and exudation along the vessels were seen in the superior nasal retina. Few perivascular sheathings were found in peripheral retina without obvious bleeding and exudation in left eye.
Few perivascular sheathings were found in peripheral retina without obvious hemorrhage and exudation in left eye (Fig1. E-H). CMV-DNA was detected in the blood and urine, while blood CMV-IgM was weakly positive. CD4 T-cell count was 24/μl. Based on these findings, a diagnosis of fulminant CMV retinitis was rendered. Intravenous antiviral therapy and intravitreal injection of antiviral medication were recommended. Due to higher risk and more financial burden of intraocular injection, only Intravenous antiviral therapy was administered.. Subsequently, we gave her ganciclovir 5 mg/kg intravenous drip 2/d. The baseline laboratory results were listed as the followings: neutrophil count of 3.9×109/L, hemoglobin of 125g/L, platelets of 177×109/L, and creatinine of 196μmol/L.
After a week, her best corrected visual acuity was 20/100 in the right eye (OD) and 20/25 in the left eye (OS). Funduscopic examination revealed perivascular sheathing in right eye was reduced. Diffuse punctuate exudation was seen in pole retina. Hemorrhage and exudation were disappeared. A small number of granular lesions were seen in the peripheral retina (Figure 2. A-D). Perivascular sheathings in peripheral retina of left eye were lighter (Figure 2. E-H). Her CD4 T-cell count was 64/μl. Her fundus lesions diminished significantly and CD4 T-cell count increased.
Figure 2: Fundus findings at 1-week reexamination (A-D: right eye, E-H left eye): Funduscopic examination revealed perivascular sheathing in right eye was much less than before. Diffuse punctate exudation was seen in pole retina. Hemorrhage and exudation were absorbed. A small number of granular lesions were seen in the peripheral retina. Perivascular sheathings in peripheral retina of left eye were less than before.
Therefore, the current systemic treatment continued. The patient was followed up every week for eye examination. Blood CD4 T-cell count, complete blood count, liver and kidney function were monitored. CD4 T-cell count increased. Her vision and fundus condition continuously improved.. Therefore, we reduced ganciclovir dosage to 5 mg/kg intravenous drip 1/d in the fourth week. After six weeks, her best corrected visual acuity was 20/50 in the right eye (OD) and 20/25 in the left eye (OS). Funduscopic examination revealed perivascular sheathing in right eye was degraded. Fewer exudations wasseen in pole retina. Hemorrhage and exudation were absent. Scarring of retinal focus and a small number of granular lesions was present (Figure 3. A-D). Perivascular sheathings in peripheral retina of left eye disappeared (Figure 3. E-H). Her CD4 T-cell count was 147/μl. Follow up at 4 mouths, her best corrected visual acuity was 20/20 in both eyes. Funduscopic examination revealed no perivascular sheathing in both eyes. Retinal focus of right eye showed healing scar. The blood vessels were white (Figure 4. A-H). The CD4 T-cell count was 254/μl. Systemic antiviral medication discontinued. There was no evidence of recurrence in 6 months of follow-up.
Figure 3: Reexamination of fundus (A-D: right eye, E-H: left eye): Funduscopic examination revealed perivascular sheathing in right eye was degraded. Few exudations were seen in pole retina, bleeding and exudation were absorbed than before, scarring of retinal focus, a small number of granular lesions was present. Perivascular sheathings in peripheral retina of left eye were not seen.
Figure 4: Four months after reexamination, fundus findings (A-D: right eye, E-H: left eye): Funduscopic examination revealed no perivascular sheathing in both eyes Retinal focus of right eye was scared and the blood vessels were white.
DISCUSSION
CMV infects the eye hematogenously and cuases retinaldiseases. Variable degrees of retinal edema lead to pale areas of the retina. Histologically, CMV retinitis exhibits areas of fullthickness retinal necrosis and edema or exudation. Clinically, CMV retinitis can be divided into two different types [5], fulminant or edematous retinitis and slow or nodular retinitis.Histologically, fulminant or edematous retinitis shows wedgeshaped areas of whitening with associated dense hemorrhage and edema. and retinal vasculitis with perivascular sheathing (an atypical manifestation with clinical appearance similar to frosted branch angrites) [6]. while slow or nodular retinitis displays inconspicuous edema, light retinal turbidity, granular focus, few fusions, less or no retinal hemorrhage, and no vascular sheath formation, which often appears in the peripheral retina[7]. CMV retinitis is a clinical diagnosis, based on the classic clinical presentations in susceptible individuals. Clinicall, CMV infection occurred in both eyes and retinal perivascular sheathing is the most prominent sign in fundus, with regional peripheral omental hemorrhage edema. A diagnosis of CMV retinitis is rendered based on the abovementioned clinical manifestations in conjunction with CMVDNA positivity in blood and urine samples. Therefore, CMV retinitis can be diagnosed in immunocompromised children, based on the clinical manifestations and other supportive laboratory results, when intraocular fluid is not available.
CMV specifically infects T lymphocytes.CMV retinitis is closely associated with the CD4 T-cell counts, which can be used to predict the risk of CMV retinitis [8]. In addition to regular monitoring visual acuity and fundus manifestations in CMV retinitis patients, the count of CD4 T-cell should be detected simutaneously. Therefore, we recommend that CD4 T-cell count should be measured when regular eye examination is performed after acute lymphoblastic leukemia chemotherapy. We should be on highly cautious of CMV retinitis for the patients whose CD4 T-cell count is low, especially less than 100 /μl, and CMV-DNA is detected.
In our patient, after early diagnosis and early systemic administration of ganciclovir antiviral medication,, CMV retinitis was well controlled.. However, the antiviral therapy of ganciclovir may cause toxicity to other organs. Therefore, the use of intravitreal injection for the treatment of CMV retinitis is recommended. General anesthesia is needed for younger patients to administer intravitreal injection. Both financial cost and risk of complications are high. Unlike our case, it has been reported that the change of perivascular sheathing in the fundus of children with CMV retinitis is rare, and the prognosis is poor. [9]
In summary, CMV retinitis is not uncommon in acute lymphoblastic leukemia pediatric patients who receive chemotherapy only, especially in the maintenance stage. With routine follow-up, early diagnosis and intravenous antiviral therapy, these patients have a good prognosis.
REFERENCES
1. Buxmann H, Hamprecht K, Meyerwittkopf M and Friese K (2017) Primary Human Cytomegalovirus (HCMV) Infection in Pregnancy. Dtsch Arztebl Int 114(4): 45-52.
2. Zambarakji H, Newson R and Mitchell S (2001) CMVR diagnoses and progression of CD4 cell counts and HIV viral load measurements in HIV patients on HAART. Br J Ophthalmol. 85(7): 837.
3. Singh R, Singh R, Trehan A, Jain R, et al. (2013) Cytomegalovirus Retinitis in an ALL child on exclusive chemotherapy treated successfully with intravitreal ganciclovir alone. J Pediatr Hematol oncol 35(3): e118-e119.
4. Baumal CR, Levin AV and Read SE (1999) Cytomegalovirus retinitis in immunosuppressed children. Am J Ophthalmol 127(5): 550-558.
5. Holland G (1996) Cytomegalovirus diseases. Ocular Infection & Immunity.
6. Listed N (1997) Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial: 5. Clinical features of cytomegalovirus retinitis at diagnosis. Studies of ocular complications of AIDS Research Group in collaboration with the AIDS Clinical Trials Group. Am J Ophthalmol 124(2): 141-157.
7. Henderly DE, Freeman WR, Causey DM and Rao NA (1987) Cytomegalovirus retinitis and response to therapy with ganciclovir. Ophthalmology 94(4): 425-434.
8. Biswas J and Sudharshan S (2008) Anterior segment manifestations of human immunodeficiency virus/ acquired immune deficiency syndrome. Indian J Ophthalmol 56(5): 363-375.
9. Fine HF, Smith JA, Murante BL, Nussenblatt RB, et al. (2001) Frosted branch angiitis in a child with HIV infection. Am J Ophthalmol 131(3): 394-396.