Previous Issues Volume 8, Issue 4 - 2024
Comparison of the Effectiveness of Platelet-Rich Fibrin and Hyaluronic Acid Injections on the Pain Management of Temporomandibular Joint Disorder
Montoya Luis G1,*, Merchan Mariangel1, Mora Oscar Augusto1-3, Gutiérrez Gabriel1
1Dentist, Faculty of Dentistry, University of Carabobo, Valencia, Venezuela.
2Specialist in Oral Surgery Central University of Venezuela, Venezuela.
3Maxillofacial Surgery Care Residence, Ángel Larralde University Hospital, Carabobo, Venezuela.
*Corresponding Author: Luis Gerardo Montoya Davila. Dentist (DMD), Faculty of Dentistry, University of Carabobo, Valencia, Venezuela. Imaging Technologist, University Arturo Michelena, San Diego, Venezuela. Mailing Address: 5501 Glenridge Dr, Atlanta, Georgia-30342, USA. Tel: +1 (857) 347-1289, ORCID: 0000-0001-8332-2424, Email: [email protected]
Received Date: November 06, 2024
Published Date: December 02, 2024
Citation: Montoya LG, et al. (2024). Comparison of the Effectiveness of Platelet-Rich Fibrin and Hyaluronic Acid Injections on the Pain Management of Temporomandibular Joint Disorder. Mathews J Dentistry. 8(4):55.
Copyrights: Montoya LG, et al. © (2024).
ABSTRACT
Background: There are different treatments for painful temporomandibular joint dysfunction (TMD), one of them is intra- articular injection in moderate to severe cases. Purpose: The study aimed to compare the effectiveness of the use of platelet-rich fibrin and Hyaluronic Acid injections to treat painful TMD, both accompanied by traditional treatment with an occlusal splint (OS). Study Design, Setting, Sample: This is a prospective, quasi-experimental research study with a pretest-posttest with a control group design. A non-probabilistic sample was taken with subjects recruited from authors' private practices from June 2023 to September 2023. The eligibility criteria for this study were adults with pain level at the TMJ equal or higher than 6 according to the Numerical Pain Rating Scale (NPRS). Predictor/Exposure/Independent Variables: The predictor variables were the injection treatments using Platelet Rich in Fibrin in conjunction with OS and Hyaluronic Acid in conjunction with OS. These were randomly assigned to subjects, each one of them representing a group for comparison purposes. Main Outcome Variables: Painful dysfunction was evaluated using the NPRS scale reported by subjects in-person visits throughout the 45 days treatment. Covariates: Demographic variables such as age and sex were considered for this study. Analyses: Descriptive data were represented using mean and standard deviation (SD). The data was compared using ANOVA test with statistical significance situated at <0.05. This was accompanied by Post Hoc analysis. Results: The study sample consisted of 60 subjects divided into three groups: PRF group with OS, HA group with OS, and OS by itself as the control group. 76% were female and with a mean age of 38 ±15.85. The results obtained showed the PRF in conjunction with OS treatment was the most effective; achieving a pain resolution within the 1st appointment in 70% of the subjects tested. Statistical significance was found in this regard among groups (F = 0.212 and P value = 0.000). Conclusions: While all treatments relieve the painful symptoms of the TMJ dysfunction, the PRF plus OS is the most effective and has the best, fastest results in resolving pain.
Keywords: Temporomandibular Joint Disorders, Platelet- Rich Fibrin, Hyaluronic Acid, Occlusal Splints.
INTRODUCTION
The temporomandibular joint (TMJ), is the type of diarthrotic joint, better defined as a ginglymoarthrodial, multiaxial, synovial, bilateral, bicondylar and simultaneous joint [1,2]. Temporomandibular disorders (TMD) are the most common cause of pain and dysfunction in the orofacial region and are related to symptoms in areas such as the head, ears, and cervical spine. At the epidemiological level, data indicates that approximately 40-60% of the population has at least one symptom of stomatognathic system dysfunction [3]. This high prevalence is related to its multidimensional etiology, lack of knowledge on behalf of dental professional about their management, diagnostic and therapeutic difficulties [3,4].
The Painful TMD, is one of the most common forms associated to TMD, affecting 10% of the world's population with a high prevalence in young women. The dysfunction can cause difficulty in chewing, clicking when opening and closing the jaw, pain, discomfort, and locking of the jaw joint. Treatments include pharmacological therapies, muscle injections, minimally invasive joint injections and surgical procedures [5-7].
Currently, the intervention of a multidisciplinary team such as a psychologist, behavioral therapist, kinesiologist and/ or physiotherapist, along with the dentist, is considered necessary to reduce painful symptoms in those patients with high rates of stress reactivity associated with psychological and psychosocial factors. There are alternatives to minimize painful dysfunction conservatively such as physical physiotherapy, localized steam application, therapy occlusal appliances, among others. On the other hand, more invasive and aggressive surgical treatments include usually meniscoplasty and meniscectomy with replacement of the articular disc [7,8].
The occlusal splint has proven to be a fundamental treatment by relieving pain, helping in mandibular function, mitigating damage to periodontal fibers, reducing levels of cellular hypoxia of the TMJ and the protection of dental components [7-9]. The muscle relaxant plate or OS is the first-choice treatment and has shown excellent clinical results, however, it has revealed certain limitations in cases of moderate to severe pain (greater than 6, Numerical Pain Rating Scale NPRS), which do not respond effectively to reduction of pain when using it without any adjuvant treatment [9].
One of the minimally invasive treatments used today is intra-articular injection of the TMJ. This has been used as a single procedure, often associated with others, such as arthrocentesis or arthroscopy, obtaining good results. Greater effectiveness of intra-articular injections with substances such as hyaluronic acid and fibrin-rich fibrin has been demonstrated. These contribute to pain relief and improve symptoms of TMD. They are considered even less invasive treatments compared to arthrocentesis [10].
However, there is no single or established “Gold Standard” protocol for the management of this pathology. Hyaluronic acid (HA) injection is widely used to treat this type of pathology or alterations of the TMJ. It is an elastoviscous fluid secreted naturally within the joint by chondrocytes and synoviocytes, whose main function is to restore or replace the synovial fluid [11].
The therapeutic properties of HA are based on its mechanical and metabolic action. The mechanical action is associated with lubrication and, consequently, less wear of the articular surfaces with reduced friction within the intra-articular space. Its metabolic action consists of facilitating nutrition in avascular areas of the articular cartilage, which improves the physiological functioning of the joint [12]. Generally, in TMJ dysfunctions, the increase in low molecular weight Hyaluronic Acid (HA) is the direct cause of decreased synovial fluid viscosity [13].
On the other hand, platelet-rich fibrin (PRF) is an immune and platelet system. Significant benefits to healing and immunity have been demonstrated. Its architecture appears to be responsible for the slow release of Growth Factors (GF) and matrix glycoproteins (≥7 days - up to 28 days) and play an essential role in PRF biology [14,15].
Literature suggests that PRF injection could improve joint conditions, not only with the expansion of the joint cavity but also due to its ability to restore the disc, capsule and retrodiscal pad and inhibit pro-inflammatory cytokines. The PRF has a high capacity to release large concentrations of several growth factors, such as prostaglandin growth factor (PDGF), transforming growth factor beta (TGF-b) and collagen [16,17].
In this sense, the objective of this study is to compare the effectiveness of the use of Platelet-rich fibrin and Hyaluronic Acid injections, alongside occlusal splint, in the treatment of painful temporomandibular joint dysfunctions.
MATERIALS AND METHODS
Study design and Sample
This was explanatory prospective research. It had a pre- and post-test design with a control group. The population consisted of adults living in Carabobo, Venezuela from June 2023 to September 2023. A convenience sample was taken, and it consisted of research subjects who attended private consultation and were divided into three groups. The treatment selection for each subject was random. Inclusion criteria used for this sample were adults, men and women aged 18-75 years, with pain level at the TMJ equal or higher than 6 according to the Numerical Pain Rating Scale (NPRS). Subjects had to be healthy at the oral and/or dental level. Exclusion criteria managed were study subjects with pain levels below 6; age outside the determined range; and presence of pain related to dental and oral pathologies, trauma, cysts, or tumors. Subjects with systemic diseases but otherwise with good oral health, were treated in this study, however, subjects with poor oral health were excluded.
Variables
The predictor variables
We used two injection treatments accompanied using occlusal splint, and the splint alone for the control group which compares Dr. Mora's protocol [18]. The first group received injections with 1% hyaluronic acid (Viscoplus, Biomedical). It is of synthetic origin, its presentation comes in 2mL, and its molecular weight is 2.5 million Daltons. The second group received injections with platelet-rich fibrin, prepared from each subject's blood. For this purpose, venipuncture is required. In the treatment appointment four test tubes are filled with the subject's venous blood. The tubes are taken to the centrifuge at 4000 rpm for 10 minutes to separate the blood clot form the platelet-rich fibrin. After the membrane separates, the liquid portion is collected (injectable PRF) and injected into both joints. The injections were 0.6cc for HA and PRF. The protocol established three injections in which the first one is in both TMJ and the other two were only in the most affected TMJ. Considering that they must be applied every two weeks, no more injections were applied, and subjects were left for observation for 6 months using the occlusal splint at night. For the injection procedures, asepsis and antisepsis measurements are taken on the articular surfaces; then, the surgeon marks the area in front of the tragus and the patient must be in maximum mouth opening to palpate the posterior edge of the mandibular condylar process and proceed to inject the solutions.
The occlusal splint (OS) was used by experimental groups post-injection and as only treatment for the control group. After the subject agreed to receive treatment, anatomical impressions were taken to create a rigid acrylic occlusal splint. It was adapted with at least 12 points of contact when biting. The subject was instructed to use it for 15 days during the morning, afternoon, and night, except when eating. Subsequently, the use was reduced after the second appointment to only two shifts, morning or afternoon and mandatorily at night. After the third appointment, the OS was indicated for use only at night. In all cases, the indication for the OS was projected to last approximately 6-12 months or until joint pain symptoms cease. The occlusal splint's design was rigid made of acrylic, and it was only used in the maxilla from the first right upper molar to the first left upper molar with canine guidance on both sides and a minimum of twelve contact points. Patients that were using removable dental prostheses were supposed to wear it at night and remove it throughout the day, which accomplished the same results as the occlusion splint. Sixty subjects were selected from a pool of both women and men between the ages of 18 and 74 with good oral health and painful symptoms in the TMD. The treatment decision was randomly assigned.
Outcome Variables
The outcome variable is Painful dysfunction. It was evaluated using NPRS scale during four consults in a 45-days treatment period. The scale consists in numerical values from 0 to 10 placed on a straight line, with 0 being the absence of pain and the value of 10 being the maximum pain reported by the subject. The derived ranges are called mild pain (1-3), moderate pain (4-6), severe pain (7-9), and very severe pain (10). This allowed us to handle this variable as a continuous type for analyses. The pain scale was recorded four times during the experiment: First appointment before applying the treatment, a 2nd appointment 15 days after the injection, a 3rd appointment 30 days after, and 4th appointment 45 days after the procedure.
Covariates
Demographic variables age and sex were considered. They were used to give contrast to the results obtained and further analyze data in search for possible patterns.
Data collection methods
For each subject, the following protocol was followed: initially, the clinical record was filled out, followed by pain estimation. This in conjunction with a radiographic analysis and clinical evaluation to rule out any pathology associated with the oral region and to make an accurate diagnosis compatible with painful dysfunction of the temporomandibular joint. Subsequently, the treatment alternative and the procedure to apply it were explained to the patient. After obtaining an informed consent, the creation of the OS followed and adapted in the next appointment. The injections started in the following appointments as explained previously as part of Dr. Mora's protocol.
The recordings of pain estimations expressed by the subjects were done in person at each appointment using a guide designed for that purpose. The treatment was started by attending to the principles of bioethics and biosafety. Subjects provided their informed consent, which implied being aware of the treatment that they were going to be subjected to and publishing the study findings for research purposes. No personal identifying information was included to protect patient privacy.
The protocol and all study procedures were evaluated under the regulations of the bioethics and biosafety operational commission of the Dentistry Faculty of Carabobo University under control number COBB/Teg:025.
Data analysis
Descriptive and inferential analyses were performed. Data was grouped in frequencies, absolute and relative, and studied using mean and standard deviation. All information was tabulated and graphed for comparison between all groups. Groups were compared through using the ANOVA test with a confidence interval of 95% and a statistical significance situated at P<0.05. This was accompanied by Post Hoc analysis. The SPSS program for Windows version 11.0 was used in this study (Figures 1-4).
Figure 1. Intra-articular puncture of injectable PRF.
Figure 2. Removal of needle from the patient.
Figure 3. Viscoplus Hyaluronic Acid 1% 2mL synthetic origin.
Figure 4. Intra-articular puncture of HA.
RESULTS
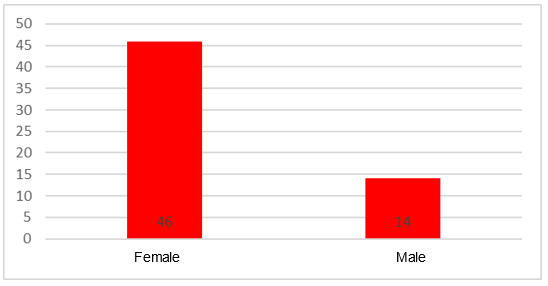
It is evident that most of the patients treated in this study (Table 1) (Graph 1) belong to the female sex with 76.67% while the male sex just represents 23.33%.
Table 1. Gender frequency distribution belonging to the sample group of Dr. Oscar Mora's private office June-September 2023
|
Gender |
Frecuency |
% |
Valid percentage |
Accumulated percentage |
|
Male |
14 |
23,3 |
23,3 |
23,3 |
|
Female |
46 |
76,7 |
76,7 |
100 |
|
Total |
60 |
100 |
100 |
Graph 1. Gender frequency distribution Data obtained from Table 1.
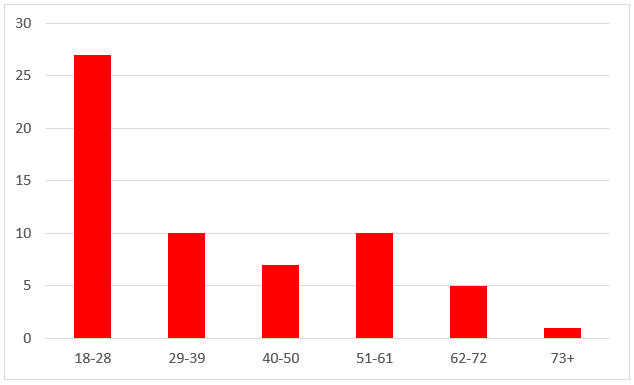
Analyzing the sample (Table 2) (Graph 2), we realized that it was distributed in the following way, that the majority or 45% of the sample was made up of people between 18-28 years of age, followed by the groups of 29-39 years of age and 51 -61 years of age by 10% each, remaining stable in the distribution of the other groups. The minimum age range being 18 years old and the maximum age being 73 years old.
Table 2. Gender frequency distribution belonging to the sample group of Dr. Oscar Mora's private office June-September 2023
|
|
Nº |
Average |
Standard deviation |
Min |
Max |
|
Age |
60 |
38.02 |
15.85 |
18 |
73 |
Graph 2. Age frequency distribution. Data obtained from Table 2.
All the 60 patients were taken as a sample; all completed the study according to the established protocol.
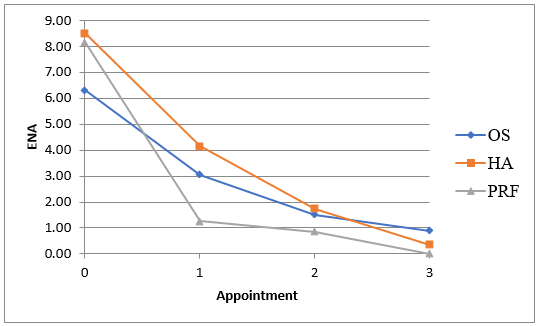
The graph of mean pain intensity (Table 3) (Graph 3) shows a more pronounced decrease in pain in the group treated with PRF from appointment No. 1 compared to the other groups. A trend that was maintained until the treatment was completed since there was a resolution of the painful symptoms in these patients, which is evident in an almost absolute value of 0.10 according to the NPRS.
Table 3. Average value of Pain Intensity between appointments with the three treatments applied belonging to the sample group of Dr. Oscar Mora's private office June-September 2023
|
Appointment |
Occlusal Splint (OS) |
Standard deviation |
Hyaluronic acid (HA) |
Standard deviation |
Platelet-Rich Fibrin (PRF) |
Standard deviation |
|
Previous |
6.30 |
1.17 |
8.5 |
0.76 |
8.15 |
1.39 |
|
Quote 1 |
3.05 |
2.58 |
4.15 |
1.18 |
1.25 |
2.43 |
|
Quote 2 |
1.50 |
2.21 |
1.75 |
1.37 |
0.85 |
1.69 |
|
Quote 3 |
0.90 |
1.85 |
0.35 |
0.81 |
0.10 |
0.31 |
Graph 3. Average value of Pain Intensity between appointments with the three treatments applied belonging to the sample group. Data obtained from Table 3.
The first group with platelet-rich fibrin (PRF) with OS produced an absolute absence of pain in 70% of the sample (Table 4), 15 days after intra-articular injection, later 45 days after 90%. of absolute absence of pain and 10% of the sample remaining with mild pain once the protocol was completed.
Table 4. Pain scale-percentage of the Platelet-Rich Fibrin (PRF) group during treatment
|
Pain Scale |
Appointment |
% |
Quote 1 |
% |
Quote 2 |
% |
Quote 3 |
% |
|
Absence (0) |
0 |
0 |
14 |
70 |
15 |
75 |
18 |
90 |
|
Mild (1-3) |
0 |
0 |
3 |
15 |
3 |
15 |
2 |
10 |
|
Moderate (4-6) |
3 |
15 |
1 |
5 |
2 |
10 |
0 |
0 |
|
Intense (7-10) |
17 |
85 |
2 |
10 |
0 |
0 |
0 |
0 |
|
Total |
20 |
100% |
20 |
100% |
20 |
100% |
20 |
100% |
The hyaluronic acid (HA) group obtained a decrease in the average pain intensity of the sample (Table 5), to moderate pain 15 days after intra-articular injection by 75% compared to the average initial value. After 45 days after intra-articular injection, there is an absolute absence of pain in the 80% sample and the remaining 20% with mild pain once the protocol is completed.
Table 5. Pain scale-percentage of Hyaluronic Acid (HA) group during treatment, belonging to the sample group
|
Pain Scale |
Appointment |
% |
Quote 1 |
% |
Quote 2 |
% |
Quote 3 |
% |
|
Absence (0) |
0 |
0 |
0 |
0 |
6 |
30 |
16 |
80 |
|
Mild (1-3) |
0 |
0 |
5 |
25 |
12 |
60 |
4 |
20 |
|
Moderate (4-6) |
0 |
0 |
15 |
75 |
2 |
10 |
0 |
0 |
|
Intense (7-10) |
20 |
100 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Total |
20 |
100% |
20 |
100% |
20 |
100% |
20 |
100% |
Finally, the group with the upper occlusal splint produces a decrease in the average pain intensity of the sample to moderate pain (Table 6), 15 days after starting treatment by 35% compared to the average initial value. After 45 days after intra-articular injection, there is an absolute absence of pain in the 60% sample and the remaining 35% with mild pain once the protocol is completed.
Table 6. Pain scale-percentage of the Oclussal splint group during treatment belonging to the sample group
|
Pain Scale |
Appointment |
% |
Quote 1 |
% |
Quote 2 |
% |
Quote 3 |
% |
|
Absence (0) |
0 |
0 |
3 |
15 |
11 |
55 |
12 |
60 |
|
Mild (1-3) |
0 |
0 |
8 |
40 |
6 |
30 |
7 |
35 |
|
Moderate (4-6) |
12 |
60 |
7 |
35 |
2 |
10 |
0 |
0 |
|
Intense (7-10) |
8 |
40 |
2 |
10 |
1 |
5 |
1 |
5 |
|
Total |
20 |
100% |
20 |
100% |
20 |
100% |
20 |
100% |
Under the assumption that the recommended criteria have been applied in the design of experiments to compare the effectiveness of three treatments in pain control, based on tests of equality of the means through the study of the variance of the results known as ANOVA (Analysis of Variance) (Table 7).The values of F = 0.212 and Sig = 0.000 of the Test are statistically significant (less than 0.05), which is why the null hypothesis that the 3 or more groups behave in the same way with respect to the population mean is rejected. , that is, at least a pair of means differ.
Table 7. Anova test for the data on Pain Intensity with the three treatments, belonging to the sample group of Dr. Oscar Mora's private practice June-September 2023
|
|
Sum of squares |
gl |
Square mean |
F |
Sig. |
|
Inter-groups |
85.733 |
2 |
42.867 |
9.212 |
0.000 |
|
Infragroups |
265.250 |
57 |
4.654 |
|
|
|
Total |
350.983 |
59 |
|
|
|
Levene's test is statistically significant p=0.011, normality is rejected, if the probability associated with the normality contrasts, that is, the Kolmogorov-Smirnov-Lilliefors p-value (n>30 or 50), is less than 0.05, therefore, the alternative hypothesis. In Tukey's POST-HOC test it was evident that the behavior of the PRF differs from the other study groups.
The values of F=).212 and Sig = 0.000 of the Test are statistically significant (less than 0.05), so the null hypothesis is rejected, about the 3 groups behave in the same way with respect to the population mean, that is, at least one group of means differ.
DISCUSSION
An aspect that is important to highlight is that most of the patients treated in this study, belong to the female sex (76.6%), which shows that painful symptoms affect women 4:1 more than men, even with a greater tendency to chronicity. A fact that is confirmed in the article by D. Torul [19], with 54 patients, of which 52 were women. It can be attributed to certain factors such as anatomical and physiological differences, and psychopathological aspects. According to age, it is evident that the predominant group in said study is 18-28 years old, with an average of 38 years, compared to Deregibus [20], where the predominant group in his study was 22 to 56 years old. Over the years, there is an increase in the frequency of painful symptoms of the temporomandibular joint in the young population.
Referring to the use of platelet-rich fibrin, many investigations differ from the present one in terms of time for pain resolution. After 15 days there was a significant change, and the sample studied showed 80% absence of pain. On the contrary, the study by Albilia [5] had a significant difference in the time taken to achieve analgesia. Significant changes were obtained in the presence of pain, but after 8 weeks and 3, 6 and 12 months without absolute resolution of the painful condition. Possibly, this was due to the PRF collection method used (centrifugation was 700 rpm for 3 minutes) and the lack of an adjuvant treatment such as OS compared to the present investigation, which helped to obtain greater effectiveness in the management of PRF as a result. painful TMD.
On the other hand, the PRF sample with OS achieved a statistically significant reduction in pain intensity in less time, with a clear difference with the HA groups with myorelaxant plate and the one with only use of OS. This is due to the ability of PRF to block biological activators and signals of inflammatory factors such as proinflammatory cytokines, interleukins, interferons, tumor necrosis factor alpha, among others, which are found within the synovial membrane [21].
In the study carried out by Ghoneim [15], they found that the use of PRF in arthrocentesis was much more effective in reducing pain than the use of lactated ringer's solution. Similar case, in the study carried out by Esra, Y [22], they obtained a better result in the group that underwent arthrocentesis with PRF compared to arthrocentesis with HA and arthrocentesis alone.
Also, it was possible to verify the use of PRF and OS as a more effective method in the resolution of painful TMJ dysfunction, a relationship that our work has with the study published by De Sousa [23], they evaluated that the group injected with PRF obtained the best results at six months, while patients treated with HA or betamethasone obtained the best results at the end of the first week. The appointment protocol they used in their research at 1 week, 1 month and 6 months, and the OS was the conventional one.
Now, the use of hyaluronic acid (HA) with an OS, following Dr. Mora's protocol carried out in said research, revealed a significant decrease in pain in the different stages of the study, reaching 45 days from the beginning of the treatment. observed the absence of pain or mild pain in the patients in the sample. In comparison, the study carried out by Batifol [24] obtained, after treatment for 6 months, the absence of pain in most of the sample, but with the persistence of some cases with moderate pain. This suggests that treatment in conjunction with the OS enhances the therapeutic effect of HA, which would explain pain relief in less time, making the treatment more effective [18].
On the other hand, the effectiveness of OS in reducing myofascial pain in relation to temporomandibular disorders was evaluated by Deregibus [20]. They found that there were no significant differences between upper and lower occlusal splints at 6 months and suggested a multifactorial treatment. In contrast, the present findings show significant differences between each study group after 15 days post injection, possibly due to the non-replacement of the inflammatory environment within the TMJ, which is achieved with the injection of viscosubstitutes or viscoregenerative agents, achieving improvement in less time.
CONCLUSION
It was determined that all three alternative treatments are effective in alleviating painful TMD symptoms. The PRF with PM group was the most effective out of the three alternatives, followed by the HA with OS group, which achieved painful TMJ symptoms resolution in a shorter period. The muscle relaxant plaque is considered an adjuvant treatment that could enhance the anti-inflammatory and analgesic effects, thus, turning out to be more effective when used in combination of minimally invasive infiltrative therapies of the TMJ with PRF and HA. There are numerous alternative treatments, however, intra-articular injections are recommended as they have proven to be effective in pain management. Effective management of this pathology requires a multidisciplinary approach which must include professional oversight from specialists in other areas such as orthodontists, neurologists, otorhinolaryngologists, psychologists and psychotherapists to ensure a successful differential diagnosis. Intra-articular infiltration should be performed exclusively by qualified oral and maxillofacial surgeons.
AUTHORS CONTRIBUTIONS
Montoya Luis: A, B, C, D, E, F, H, I, J, K.
Merchan Mariangel: A, B, C, D, E, H, I, J, K.
Mora Oscar: A, B, C, E, I, J, K.
Gutiérrez Gabriel: A, C, D, F, H, I, J, K.
|
(*) Contributions to authorship in the article: |
|
|
A.Participed in the conception or design of the study |
G.Obtained financing |
|
B.Literature review |
H.Provided statistical advice |
|
C.Participed in the contribution of study material |
I.Drafting of the article |
|
D.Provided technical advice |
J.Critical review of the article |
|
E.Collection of data |
K.Approval of the final version of the article |
|
F.Analysis and interpretation of results |
L.Others, specify |
None.
CONFLICTS OF INTEREST
There are no conflicts of interest in the agreed parts of the research.
REFERENCES
- Fuenzalida R, Hernández C, Pérez J. (2017). Structural and functional alterations of the stomatognathic system: Speech therapy management [bibliographic study]. Areté issn-l:1657-2513. 17(1):29-35.
- Bordoni B, Varacallo M. (2024). Anatomy, Head and Neck, Temporomandibular Joint. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538486/
- Urbański P, Trybulec B, Pihut M. (2021). The Application of Manual Techniques in Masticatory Muscles Relaxation as Adjunctive Therapy in the Treatment of Temporomandibular Joint Disorders. Int J Environ Public Health Res. 18(24):12970.
- Rezaie K, Amiri A, Ebrahimi E, Shirani G, Salehi S, Alizadeh L. (2022). The Efficacy of Neck and Temporomandibular Joint (TMJ) Manual Therapy in Comparison with a Multimodal Approach in the Patients with TMJ Dysfunction: A Blinded Randomized Controlled Trial. J Islam Repub Iran. 36:45.
- Albilia J, Vizcaıno C, Weisleder H, Choukroun J, Ghanaati S. (2018). Liquid platelet-rich fibrin injections as a treatment adjunct for painful temporomandibular joints: pre-liminary results. Cranio. 38(5):292-304.
- Andre A, Kang J, Dym H. (2022). Pharmacologic Treatment for Temporomandibular and Temporomandibular Joint Disorders. J Oral Maxillofac Surg North Amer. 34(1):49-59.
- Ramalingam S, Saravana P. (2022). Occlusal splint therapy in TMD pain management: A review. J Global Oral Health.
- Augurto J, Parise J, Guanoluisa R, Silva P, Mora O. (2022). Temporomandibular joint dysfunction and its association with the stress reactivity index in a hospital. KIRU. 19(1):5-11.
- Gil A, Paris A, López V, Touche R. (2018). Management of pain in patients withtemporomandibular disorder (TMD): challenges and solutions. J Pain Res. 11:571-587.
- Armijos J, Hidalgo B, Velásquez B. (2020). Efficacy of hyaluronic acid in the treatment of temporomandibular disorders. Systematic review. Av Odontostomatol. 36(1):35-47.
- Iturriaga V, Mena P, Oliveros C, Torres D, Sol M. (2018). Importance of Synovial Fluid in the Temporomandibular Joint and its Implications in Joint Pathology. International. J Morphol. 36(1):297-302.
- Tesch R, Takamori E, Calcia T, Lobo F, Leitão E, Fontes L. (2022). Platelet-Rich Fibrin for treating temporomandibular disorders in adults: A Scoping Review protocol. Int J Evid Based Healthc. 4:e4165.
- Derwich M, Mitus M, Pawlowska E. (2021). Mechanisms of Action and Efficacy of Hyaluronic Acid, Corticosteroids and Platelet-Rich Plasma in the Treatment of Temporomandibular Joint Osteoarthritis-A Systematic Review. Int J Mol Sci. 22(14):7405.
- Choukroun J, Diss A, Simonpieri A, Girard M, Schoeffler C, Dohan S, Dohan L. (2006). Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 101(3):e56-e60.
- Crisci A, Manfredi S, Crisci M. (2019). Fibrin Rich in Leukocyte-Platelets (L-PRF) and Injectable Fibrin Rich Platelets (i-PRF), Two Opportunity in Regenerative Surgery: Review of The Sciences and Literature. J Med Dent Sci. (IOSR-JDMS). 18(4):66-79.
- Ghoneim N, Mansour N, Elmaghraby S, Abdelsameaa S. (2022). Treatment of temporomandibular joint disc displacement using arthrocentesis combined with injectable platelet rich fibrin versus arthrocentesis alone. J Dent Sci. 17(1):468-475.
- Zotti F, Albanese M, Rodella L, Nocini P. (2019). Platelet-Rich Plasma in Treatment of Temporomandibular Joint Dysfunctions: Narrative Review. Int J Mol Sci. 20(2):277.
- Carrasquel K, Camacho C, Mora O. (2011). Intra-articular injection with hyaluronic acid and use of the occlusal spacer as therapy in painful temporomandibular dysfunction. Scientific Odous. 12(2).
- Torul D, Cezairli B, Kahveci K. (2021). The efficacy of intra-articular injectable platelet-rich fibrin application in the management of Wilkes stage III temporomandibular joint internal derangement. Int J Oral Maxillofac Surg. 50(11):1485-1490.
- Deregibus A, Ferrillo M, Grazia M, Chiara M, De Sire A, Castroflorio T. (2021). Are occlusal splints effective in reducing myofascial pain in patients with muscle-related temporomandibular disorders? A randomized-controlled trial. Turk J Phys Med Rehabil. 67(1):32-40.
- Xu J, Hui R, Zhao S, Li Q, C Li, Bao G, Kang H. (2023). Comparative effectiveness of hyaluronic acid, platelet-rich plasma, and platelet-rich fibrin in treating temporomandibular disorders: a systematic review and network meta-analysis. Head Face Med. 19(1):39.
- Esra Y, Nurgul K. (2020). Comparison of the Efficacy of Intra-Articular Injection of Liquid Platelet-Rich Fibrin and Hyaluronic Acid After in Conjunction with Arthrocentesis for the Treatment of Internal Temporomandibular Joint Derangements. J Craniofac Surg. 31(7):1870-1874.
- De Sousa M, Nansi B, López A, Caramelo F, Flores J, Herrero J, João M. (2020). Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study. Measurement. 56(3):113.
- Batifol D, Finiels P, Jammet P. (2018). The Effect of Intra-Articular Injection of Hyaluronic Acid on the Degenerative Pathology of the Temporo-Mandibular Joint. Glob Drug Ther. 3(1):1-4.
.png)
.png)
.png)
.png)