Current Issue Volume 5, Issue 1 - 2024
Comparison Between General and Spinal Anesthesia in The Effect On Hemodynamic Stability in Patients Undergoing Hernia Repair
Adnan Abdul Adheem Kadhim1, Haider Ahmed Jalab Salem Al-Khikani2,*, Qasim Muhammad Hamza3, Yass Khudair Habib4, Muhammad Mohsen Hussein5, Hassan Taqi Muhammad6
1General Surgery Specialty, Academic Professor of the Department of Anesthesia and Intensive Care Technologies, Al-Taff University College, Karbala, Iraq
2-5Bachelor of Anesthesia and Intensive Care Technology, Al-Taff University College, Karbala, Iraq
*Corresponding author: Haider Ahmed Jalab Salem Al-Khikani, Bachelor of Anesthesia and Intensive Care Technology, Al-Taff University College, Karbala, Iraq, Tel: 07729761444, ORCID: 0009-0008-5416-1498; Email: [email protected]
Received Date: July 23, 2024
Published Date: September 14, 2024
Citation: Kadhim AAA, et al. (2024). Comparison Between General and Spinal Anesthesia in The Effect On Hemodynamic Stability in Patients Undergoing Hernia Repair. Mathews J Anesth. 5(1):15.
Copyrights: Kadhim AAA, et al. © (2024).
ABSTRACT
Introduction: The primary focus of the staff in the anesthesia and critical care unit remains selecting the best anesthesia that poses the least risk to the patient's life. This includes adhering to protocols, protocols, strategies, and guidelines for selecting the most appropriate anesthesia. It might also be argued that the most effective and common type of anesthetic used for hernia repairs is spinal anesthesia. Aim of the study: Learn about obtaining and verifying hemodynamic stability in patients undergoing hernia repair under anesthesia. Subjects and methods: precise and current analyses of the patients who visit the Karbala hospitals Al-Hassan and Al-Hussein. We classified the 100 patients who had herniotomies into two groups based on the kinds of anesthesia spinal and general. A total of 50 patients underwent spinal anesthesia and 50 patients underwent general anesthesia. Analysis was done on the patient's blood pressure change, and pulse rate. The study examined patients between the ages of 20 and 90, splitting them into two groups for meticulous follow-up prior to, during, and following surgeries general anesthesia (GA) and spinal anesthesia (SA). Results: Our findings demonstrate that while blood pressure is more constant in SA (about 56%) compared to GA (approximately 40%), blood pressure is higher in GA (32%) and SA (24%) but lower in GA (28%) and SA (20%). Based on the results of this study, heart rate stability is higher in SA (56%) compared to GA (32%), and heart rate increase was 34% in SA and 60% in GA. While the impact of SA is more sustained, the lowered heart rate was 10% in SA and roughly 8% in GA. Conclusions: we found spinal anesthesia was more than general anesthesia in stability of blood pressure and heart rate and Minimum or normal.
Keywords: General Anesthesia, Spinal Anesthesia, Hemodynamic Stability in Anesthesia, Hemodynamic Stability Hernia Repair in Anesthesia.
INTRODUCTION
Hernia treatment plans come with a number of difficulties, including postoperative analgesic medication and anesthesia for the process. Spinal and general anesthesia techniques are used during open inguinal hernia surgery [1]. Children with hypertension are known to have end-organ damage and are at risk of developing hypertension as adults, despite the lack of research regarding the long-term effects of persistent hypertension in children [2]. Hypertension is a major risk factor for stroke, coronary artery disease, and kidney damage in adults. Monitoring for the American Society of Anesthesiologists standard involves keeping an eye on the patient's temperature, circulation, breathing, and oxygenation. It is necessary to use a second pulse oximeter to measure pre- and post-ductal oxygen saturation in addition to routine monitoring. The onset of a gradient between the pre- and post-ductal oxygen saturations may signal pulmonary hypertension exacerbation [3]. Propofol lowers systemic vascular resistance, myocardial contractility, and preload to lower arterial blood pressure. Extremes in age, heart dysfunction, and higher dosages all increase the severity of these consequences. Injection pain and infrequent thrombophlebitis About 58% of injectable users of propofol report experiencing pain [4]. While most patients' blood pressure should return to normal several months prior to surgery, modest to severe diastolic or systolic hypertension does not raise the risk of anesthesia. Acute management of mild to moderate elevations shouldn't be done in the days leading up to surgery. Increased operating risk is associated with higher blood pressure increases, which need to be carefully managed prior to surgery [5]. Since Bassini's first description of inguinal hernia repair was published in 1887, other hernia repair techniques have been published, including Shouldice, Darning, Modified Bassini, Lichtenstein mesh repair, and the more recent laparoscopic treatment. Recent times have seen an increase in the popularity of laparoscopic and Lichtenstein mesh repairs due to their rapid recovery periods and low rates of recurrence [6]. Pulmonary aspiration of stomach contents and failed endotracheal intubation are the two leading causes of maternal morbidity and death following general anesthesia. Intravenous ranitidine 50 mg or metoclopramide 10 mg, or both, should be administered to patients who have extra risk factors that make them more prone to aspiration, one to two hours before general anesthesia is induced. Morbid obesity, reflux symptoms, a potentially problematic airway, and emergency surgery performed without a voluntary fasting interval are some of these risk factors. Antacid prophylaxis against aspiration pneumonia should be administered to all patients 30 to 45 minutes before induction using 30 mL of sodium citrate. 40 mg of omeprazole taken orally as a premedication [7]. Propofol primary cardiovascular action is a reduction in arterial blood pressure brought on by a decrease in cardiac contractility, preload, and systemic vascular resistance (the inhibition of sympathetic vasoconstrictor activity). Following induction, hypotension is typically reversed by the stimulation that comes with intubation and laryngoscopy. Propofol-induced hypotension is linked to several factors, such as large dosages, fast injections, and advanced age. The typical arterial baroreflexes response to hypotension is significantly impaired by propofol [8]. When comparing sevoflurane and isoflurane mixed with 67% nitrous oxide for single vital-capacity breath inhalational induction in 67 adults, it was shown to be unsuitable [9]. The hemodynamic reactions to halothane induction and maintenance of anesthesia in 68 unplanned children aged 1-3 undergoing adenoidectomy were compared with those of sevoflurane [10]. The three anesthetic choices for open groin hernia therapy are not available for all procedures. Many conditions must be met for the perfect anesthetic method. It must be simple, as safe as possible, and have minimal postoperative morbidity. The technique must be painless for the patient, provide a swift recovery without any negative consequences after surgery, and be reasonably priced [11].
Aim of the study The failure to achieve circulatory stability for patients suffering from hernia repair under general and spinal anesthesia is what prompted us to provide clear solutions to avoid this problem and prevent all complications that reduce morbidity and mortality.
SUBJECTS AND METHODS
In this study, we take 100 patients make herniectomy operation which divided into two groups of 50 subjects each (50 general anesthesia and 50 spinal anesthesia), A data analysis was done regarding the change in blood pressers and heart rate, in this study the patients were selected from twenty years to ninety years old, then divided into two groups, the patients were divided two groups: the general anesthesia group GA and the second group spinal anesthesia group SA. we listed the things that can be monitored well in the operating room and divided them into three periods before and during and after the operation, as the information that we collected was blood pressure and the variables that accompany it, such as high or low pressure, the heart rate as well, and the accompanying highs and lows, and MAP, which is that the patient went into one of the shocks from lack of fluids or cardiac shocks, Inhaled anesthetics the It is a type of anesthesia that one should be careful of because it causes a hypotension when used, Minimum alveolar concentration (MAC) inhaled anesthetic amount that in (50%) of individuals stops movement in response to a standardized stimulus (such as surgical area). Because it replicates brain partial pressure, enables potency comparisons among drugs, and offers a benchmark for experimental assessments. Spinal anesthesia provides an alternative to general anesthesia. Although a spinal anesthetic prevents pain during surgery by numbing the lower body, those who have received one might remain conscious during the procedure. Most surgeries performed below the waist can be performed under a spinal anesthetic. An anesthetist administers a spinal anesthetic Using Bupivacaine, which is the preferred and most commonly used drug in operations. Using propofol which is the preferred and most commonly used drug for general anesthesia has the greatest effect on systemic blood pressure when compared to other induction medicines; this is due to substantial vasodilation in both arterial and venous circulations, which leads to decreases in preload and afterload. This effect on systemic blood pressure is particularly significant with age, in individuals with low intravascular fluid capacity, and after a fast injection. Because the hypotensive effects are amplified by the suppression of the usual baroreflexes response, vasodilation causes only a little rise in heart rate.
RESULTS
In this study, as indicated by the Table in Distribution of Patients to the Change in Blood Pressure, we find that blood pressure is also more stable in SA (about 56%) compared to GA (about 40%); however, blood pressure increases in GA (about 32%) and in SA (about 24%), while blood pressure decreases in GA (about 28%) and in SA (20%). Based on the data presented above, it can be concluded that spinal anesthesia has a more consistent blood pressure profile than general anesthesia.
Table 1. Distribution of patients according to the change in Blood Pressure
|
NO. OF PATIENT |
INCREASE IN HR |
REMAIN |
DECREASE IN HR |
TOTAL |
|
GA GROUP |
30 |
16 |
4 |
50 |
|
60% |
32% |
8% |
100% |
|
|
SA GROUP |
17 |
28 |
5 |
50 |
|
34% |
56% |
10% |
100% |
|
|
TOTAL |
47 |
44 |
9 |
100 |
|
47% |
44% |
9% |
100% |
Table 2. Distribution of patients according to the change in Heart rate
|
NO. OF PATIENT |
INCREASE IN BLOOD PRESSURE |
REMAIN |
DECREASE IN BLOOD PRESSURE |
TOTAL |
|
GA GROUP |
16 |
20 |
14 |
50 |
|
32% |
40% |
28% |
100% |
|
|
SA GROUP |
12 |
28 |
10 |
50 |
|
24% |
56% |
20% |
100% |
|
|
TOTAL |
28 |
48 |
24 |
100 |
|
28% |
48% |
24% |
100% |
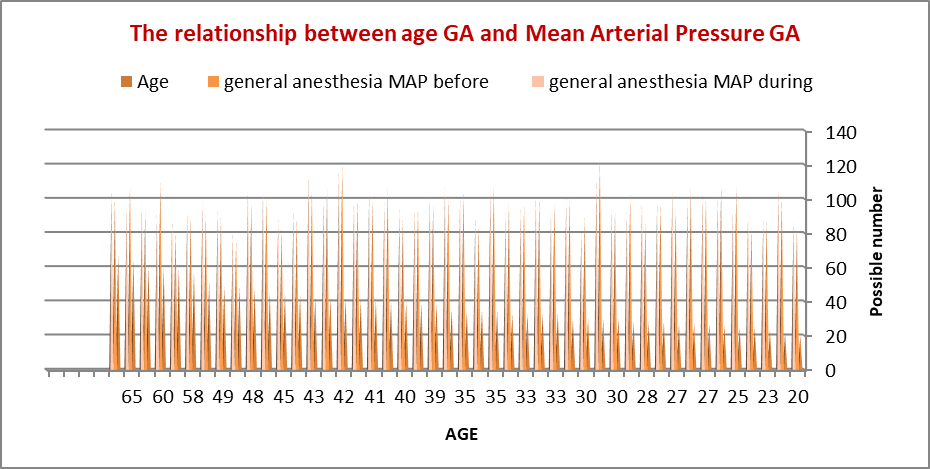
Figure 1. The Relationship between age GA and Mean Arterial Pressure GA.
that the is likewise more stable in SA (about 56%) compared to GA (approximately 40%). Without therapy, however, blood pressure increases are higher in GA (32%) and SA (24%), while blood pressure decreases are also higher in GA (28%) and SA (20%).
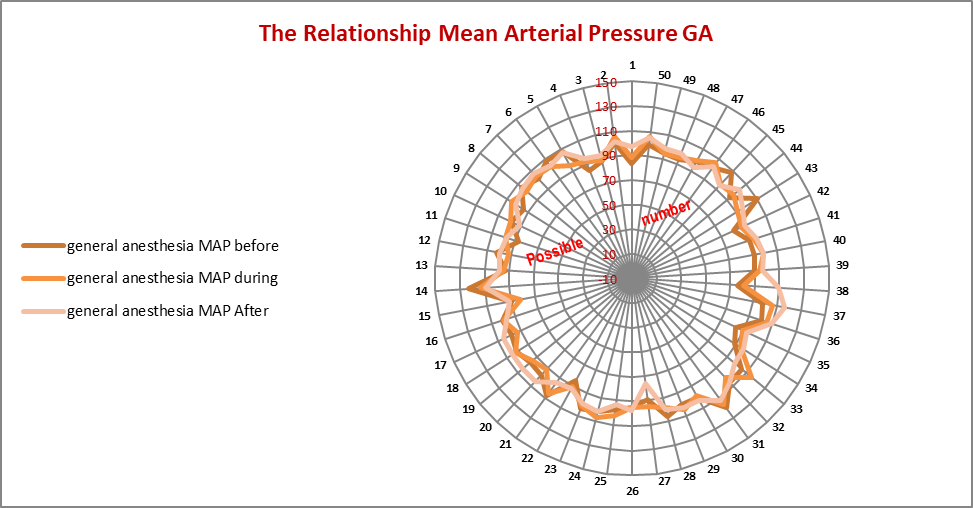
Figure 2. The Relationship Mean Arterial Pressure GA
Additionally, blood pressure in SA is more stable at roughly (56%) compared to about (40%) in GA; yet, blood pressure in GA is more likely to raise at (32%) and decrease at (28%). Thus, based on the data and statistics that are currently in front of you, it can be concluded that spinal anesthesia is superior and more stable.
DISCUSSION
Courtney J. Balentine, inguinal hernia repair is the most common general surgery procedure in the United States (15%–20%) of these procedures are performed under general anesthesia, whereby local anesthetic is used for the remaining 80% of the procedure. We postulated that as people age, there would be more benefits to local anesthetic for inguinal hernia surgery as opposed to general anesthesia [12]. Bay-Nielsen, regional anesthesia has the highest morbidity and local infiltration anesthesia has the lowest morbidity. The elective groin hernia repair procedure had a (0.12%) mortality rate within (30 days), with patients dying within a week more likely to have received regional anesthesia [13]. Anthony Rodgers, Neuraxial blocking lowers major problems such as postoperative mortality. The magnitude of some of these benefits and whether they are solely related to avoiding general anesthesia, all-cause mortality, DVT, pulmonary embolism, myocardial infarction, transfusion requirements, pneumonia, other infections, respiratory depression, and renal failure require more research [14]. David L Reich, found that severe hypotension after induction of anesthesia is quite typical, as compared to other times, it occurs more frequently in the (5–10 minute late post-induction interval). In conclusion, it is wise to think about alternatives to propofol when inducing anesthesia in patients older than (50 with an ASA physical status of III). In standard clinical practice, (9%) of patients experienced clinically significant hypotension in the first ten minutes following anesthetic induction [15]. Al-Khikani et al Owners of this research study a comparison between general and spinal anesthesia in the effect on hemodynamic stability in patients Undergoing hernia repair, having a hernia repaired, the cardiovascular system is unaffected by spinal anesthesia, which has been shown via study to be more stable than general anesthesia. Nevertheless, the benefit must be increased by precise and accurate work rather than reliance. Monitoring and correcting blood circulation abnormalities is essential.
CONCLUSIONS
We found a very noticeable increase in heart rate in general anesthesia, while spinal anesthesia was more stable, mean arterial pressure (MAP) We found a very noticeable increase in arterial pressure in general anesthesia, while spinal anesthesia was more stable, Blood pressure (PB) We found a very noticeable increase in pressure in general anesthesia, while spinal anesthesia was more stable. Achieving hemodynamic stability is crucial for balancing the supply and demand of oxygen in the heart, to achieve an identical objective, many agents and methods may be employed, includes fentanyl plus isoflurane, sevoflurane, or propofol, through a variety of mechanisms, volatile anesthetics exert cardio-protective effects [16]. The science and training are in line with the American Heart Association Guidelines Update for CPR and Emergency Cardiovascular Care, The American Heart Association's BLS course is recommended for healthcare professionals and other staff members who need to learn how to perform CPR and other basic cardiovascular life support procedures in a variety of scenarios [17]. A significant portion of individuals receiving general anesthesia are susceptible to the common occurrence of intraoperative hypotension (IH) Significant postoperative sequelae, including as renal failure, cardiac damage, and even higher mortality, are associated with the incidence of IH [18].
REFERENCES
- Callesen T. (2003). Inguinal hernia repair: anaesthesia, pain and convalescence. Dan Med Bull. 50(3):203-218.
- Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh R. (2014). Pharmacological interventions for hypertension in children. Cochrane Database Syst Rev. 2:CD008117.
- Aglio LS, Urman RD. (2017). Anesthesiology: Clinical Case Reviews. 10.1007/978-3-319-50141-3.
- Forkin KT, Nemergut EC. (2016). Miller’s anesthesia, 8th edition [Internet]. American Society of Anesthesiologists. [cited 2024 Jan 1].
- Wolfsthal SD. (1993). Is blood pressure control necessary before surgery? Med Clin North Am. 77(2):349-363.
- Mabula JB, Chalya PL. (2012). Surgical management of inguinal hernias at Bugando Medical Centre in northwestern Tanzania: our experiences in a resource-limited setting. BMC Res Notes. 5:585.
- Aitkenhead AR, Moppett I, Thompson J. (2013). Smith and Aitkenhead’s Textbook of Anaesthesia. Elsevier Health Sciences.
- Butterworth JF. (2018). Morgan and mikhail’s clinical anesthesiology. 6th ed. McGraw-Hill Education.
- Ti LK, Pua HL, Lee TL. (1998). Single vital capacity inhalational anaesthetic induction in adults--isoflurane vs sevoflurane. Can J Anaesth. 45(10):949-953.
- Meyler L, Aronson JK. (2009). Meyler’s side effects of drugs used in anesthesia. Amsterdam: Elsevier Science.
- Kingsnorth A, Leblanc KA, Sanders DL. (2018). Management of Abdominal Hernias. Cham: International Publishing.
- Balentine CJ, Meier J, Berger M, Reisch J, Cullum M, Lee SC, et al. (2021). Using Local Anesthesia for Inguinal Hernia Repair Reduces Complications in Older Patients. J Surg Res. 258:64-72.
- Bay-Nielsen M, Kehlet H. (2008). Anaesthesia and post-operative morbidity after elective groin hernia repair: a nation-wide study. Acta Anaesthesiol Scand. 52(2):169-174.
- Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. (2000). Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 321(7275):1493.
- Reich DL, Hossain S, Krol M, Baez B, Patel P, Bernstein A, et al. (2005). Predictors of hypotension after induction of general anesthesia. Anesth Analg. 101(3):622-628.
- Kaplan JA, Augustine's JGT, Manecke GR, et al, eds. (2017). Kaplan's Cardiac Anesthesia for Cardiac and Noncardiac Surgery. 7th edn. Philadelphia, PA: Elsevier. pp. 731.L -769.L.
- Pardo M. (2022). Miller’s Basics of Anesthesia. Elsevier Health Sciences.
- Benes J, Simanova A, Tovarnicka T, Sevcikova S, Kletecka J, Zatloukal J, et al. (2015). Continuous non-invasive monitoring improves blood pressure stability in upright position: randomized controlled trial. J Clin Monit Comput. 29(1):11-17.