Current Issue Volume 9, Issue 1 - 2024
Clinical Manifestation and Papilledma as Intracranial Hypertension in Behcet’s Disease without Cerebral Venous Thrombosis
Gholamhossein Yaghoobi1,*, Mohammad Dehghanifiroozabad2, Mohammadali Yaghoobi3
1Ophthalmologist, Birjand University of Medical Science, Social Determinant Health Research Center, Department of Ophthalmology, South Khorassan, Birjand, Iran
2Neurologist, Birjand University of Medical Science, South Khorassan, Birjand, Iran
3Internist, Mashad University of Medical Science, Department of Internal Medicine, Ghaem Hospital, Razavi Khorassan, Mashhad, Iran
*Corresponding author: Dr. Yaghoobi Gholamhossein, MD, Ophthalmologist, Birjand University of Medical Science, Social Determinant Health Research Center, Department of Ophthalmology, South Khorassan, Birjand, Iran, Phone: 985632626251, Email: [email protected]
Received Date: October 07, 2024
Published Date: December 11, 2024
Citation: Yaghoobi G, et al. (2024). Clinical Manifestation and Papilledma as Intracranial Hypertension in Behcet’s Disease without Cerebral Venous Thrombosis. Mathews J Ophthalmol. 9(1):37.
Copyrights: Yaghoobi G, et al. © (2024).
ABSTRACT
Introduction: Behcet's syndrome is an inflammation of vascular system it may have a clinical feature initially that lead to numerous signs and symptoms which may appeared unrelated to it at first. It could be affected the mouth sores, eye inflammation, skin lesions or genital sores. Behcet's disease have different presentation and early treatment could be reducing or prevent serious eye complications, such as blindness. To report a case of papilloedema without dural sinus thrombosis according to clinical and imaging study, diagnosis confirm by acneiform appearance therafter. Case description: A 25-year-old male, presented with a four-week history of increasingly severe headache, nausea and blurring of vision. Ophthalmic examination showed papilledema without any other ocular finding. The patients admitted in neurology ward and clinical and paracilinical study suggestion was idiopathic intracranial hypertention. The patient discharge and prescribed acetazolamid tablet to maintain lowering intracranial pressure. The patient three months latter comeback with prefund visual loss and bilateral optic atrophy that development of oftus lesion and acneiform skin lesions confirm Behcet's disease Conclusion: Although uveitis is a main clinical feature but variable presentation in Behçet's disease, such as papilledema could be considered in different diagnosis of it. The consequent of optic atrophy after three months of papilledema had great value in early suspicion of Behçet's disease to definite diagnosis and do prompt treatment in spite of any sign of cerebral venous thrombosis in this late appearing skin lesion.
Keywords: Behcet’s Disease, Papilledema, Diagnosis.
INTRODUCTION
Behcet’s disease (BD) describe first time by Hulusi Behçet, who report cases who had, oral and genital ulcers and hypopyon uveitis. The disease has been recognized since as vasculitis with multiple disease manifestations [1,2]. Behcet’s disease seen more in geographical distribution along the ancient route known as the ‘Silk Route’, extending from the Mediterranean countries to the Far East. Therefore, it is suggesting the common etiological insult, including several genetic factors such as HLA-B5 which spread through this way [3].
Papilledema is defined as optic disc edema secondary to high intracranial pressure (ICP). Hense, papilledema cannot exist in the absence of high ICP. The causes of high ICP or intracranial hypertension (IH) may be due to space occupying lesion such as brain tumor, meningitis, cerebral venous sinus thrombosis (CVT) or may be unknown as idiopathic [4,5].
The central nervous system (CNS) is the site where the neurological involvement is most likely to be encountered. The peripheral nervous system is affected which usually have a subclinical form, that is confirmed by electrophysiological studies. According to the lesions site the Neuro-Behcet’s classifying to two categories. The first is the cerebral parenchyma involvement that occur in 20%–60% of cases. It is a small inflammatory lesion in the brain stem and the basal ganglia, which should be considered in the differential diagnosis of diseases like multiple sclerosis (MS). The Sensory symptoms, movement disorders and epilepsy have been reported. It also showed two stage that acute phase has favorable to diagnosis to treatment versus the chronic form can causes brain atrophy and more aggressive course. The spinal cord can also be affected, either due to the proximity of the lesions or in an isolated manner, which constitutes a factor indicating a poor prognosis. The most common type is multifocal transverse myelitis. The second pattern have vascular involvement, basically by thrombosis of the cerebral venous sinuses, which occurs in 10%–20% of the patients. The venous system including superior sagittal and transverse sinuses could be affected. It usually presents as a syndrome of intracranial hypertension and, to a lesser extent, with focal symptoms or epileptic seizures. Cerebral infarctions are less frequent; they can simultaneously affect small and large arteries [6].
Our report was emphasized on this finding and demonstrated not only the value of many challenging spectrum of papilledema but also its modalities response to treatment and its long-term outcome which still are uncertain due to the small number of patients reported in the literature up till now.
CASE DESCRIPTION
We reported a 25-year-old male, presented with a four-week history of increasingly severe headache, nausea and blurring of vision. The patient medical history revealed that he had previous recurrent oral ulcers, without any suggestion of skin lesions and arthralgia in joint over the past two years.
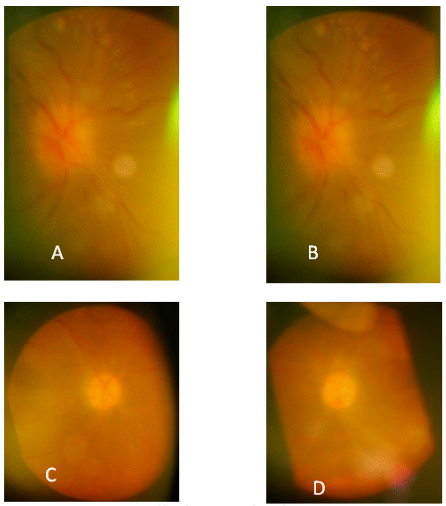
On physical examination, the vital signs were normal. Ophthalmic exam showed a best corrected visual acuity (BCVA) of 20/20 in both eyes, and full eye movement. The pupils were found to be regular and reactive with no afferent pupillary defect in both eyes. The intraocular pressure level in both eyes were in normal limit. Anterior segment examination indeed of vitreous examination dose not showed any abnormality except of bilateral papilledema without any vitreoretinal or vascular inflammation (Figure 1). Color vision and other aspects of the neurological examination were unremarkable on remainder of physical examination.
Figure 1. A&B papilledema in both eye. C&D optic atrophy 4 months later.
The non-contrast computerized tomography (CT) scan of the brain and orbit was normal. MRI of brain with and without contrasted and a magnetic resonance venography and angiography (MRV&MRA) did not show any abnormality (Figure 2).
Figure 2. A normal brain MRI, B: Normal MRI with contrast, C: Normal MRV, D: Normal MRA.
The lumbar puncture had increasing of cerebrospinal fluid pressure (CSF) of 380 mm H2O. Laboratory tests showed hemoglobin 11.1 g/dl, ESR 120 mm/hr and C-reactive protein 0.4 mg/dl. The below others test within normal or negative investigations included WBC, platelets, prothrombin time, antithrombin III, factor V, factor IX, factor XI, factor VIII, protein C, protein S, homocysteine, anticardiolipin, anti-double-stranded DNA, ANA, rheumatoid factor, liver function tests, renal function tests, lipid profile, urine analysis, sickle cell screening test, chest HLAB5, X-ray, CT scan of the chest, electrocardiogram (ECG) and echocardiogram.
Diagnosis of BD was ruled out after neurological and rheumatological consultations. The cerebrospinal fluid composition was normal so, the patient was discharge in a possible diagnosis of idiopatic intracranial hypertention.
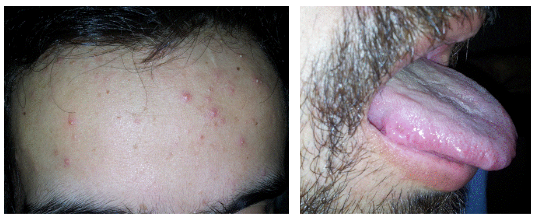
After four months the patient again admitted with severe headache, tong ulcer and acneiform skin lesions (Figure 3). Ophthalmic examination showed a best corrected visual acuity of 20/200 in both eyes. Anterior segment examination and vitreous were within normal limit except of bilateral optic atrophy without any vitreoretinal or vascular inflammation (Figure 1C&D).
Figure 3. Acneiform lesion & oral aft us.
After neurological and rheumatological consultations, a diagnosis of incomplete BD was made with intracranial hypertension. The patient was started on prednisolone 60 mg/day, warfarin 5 mg/day, azathioprine 100 mg/day, and colchicine 0.5 mg twice a day. With improvement of the headache during the first 2 weeks, Cyclosporine 100 mg/day was added subsequently and the patient was maintained on 10 mg prednisolone daily.
DISCUSSION
This case is presented with papilloedema without any attributable underlying disease primirly. The clinical,paraclinical and radiological manifestation did not fulfill the criteria for diagnosis of any accompanying diseases indeed of our suspicious to Behcet's disease. The appearance of oral ulcers and evidence of acneform skin lesion therafter was the key that strongly supported the diagnosis of incomplete Behcet's disease.
Diminished fibrinolytic activity has also been reported in the peripheral blood of patients with Behcet's disease. This may partly explain the predilection of patients with Behcet's disease to develop thrombotic events in general, and dural sinus thrombosis in particular with subsequent raised intracranial pressure and Papilledema [7]. In spit of that there is also report among Behcet's disease and high intracranial pressure [8]. Our case was not consistent with these observations because characteristically attended with papilledema without accompany other systemic or other ocular finding.
Therefore, not only the exact cause of Behçet’s disease is not clearly understood but genetic (HLA-B51, allele genetic variations, the IL-10, IL-23R, and ERAP1 genes), infections (Streptococcus sanguis and herpes simplex virus) and Innate and adaptive immune responses are involved in Behcet's disease. The more produced pro-inflammatory cytokines, such as IL-1β, IL-6, IL-17, IL-22and TNF-α involved in Behcet’s disease. So, TNF-α inhibitors (infliximab and adalimumab) and Methotrexate, azathioprine cyclophosphamide and cyclosporin also used in this multisystem disorder. the treatment approach is often individualized depending on the organs involved. Immunosuppressive medications such steroid, there were many conflicts in differentiating papilledema as describe in a case that showed a rare optic disc involvement which misdiagnosis as a papilledema [9].
There were many conflicts in differentiating papilledema as describe in a case that showed a rare optic disc involvement which misdiagnosis as a pupilledema [10]. The other study also considered in the differential diagnosis of intracranial hypertension, especially in areas where the disease prevalence is high in a known case of BD [11].
We recommended closed follow up in patients with suspect Behcet's disease which presenting with papilloedema and supported the late appearance that may be fulfilled characteristic feature later.
CONCLUSION
We reported this case to highlight the importance of including BD as a cause of papilledema, especially in a young patient that there is a high index of clinical suspicion without definite diagnostic criteria's. We also aimed to increase the awareness of neurological manifestations of BD that other criteria could be obvious later.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTERESTS
The authors declare that there is no conflict of interest.
REFERENCES
- Ronald B, McGregor L, Kenneth C. (2014). Behçet’s disease in the United States. Northeast Florida Med. 65(2):27-37.
- Hatemi I, Hatemi G, Çelik AF. (2018). Gastrointestinal Involvement in Behçet Disease. Rheum Dis Clin North Am. 44(1):45-64.
- Verity DH, Marr JE, Ohno S. (1999). Behçet’s disease, the Silk Road and HLA-B51: historical and geographical perspectives. Tissue Antigens. 54:213-220.
- Rigi M, Almarzouqi SJ, Morgan ML, Lee AG. (2015). Papilledema: epidemiology, etiology, and clinical management. Eye Brain. 7:47-57.
- Peters KS, Schuman SG, Sengupta S, Maheswaranathan M, Gospe SM. (2024). Papilledema and Combined Central Retinal Artery and Central Retinal Vein Occlusion as a Manifestation of Behçet Disease. J Neuroophthalmol. 44(3):e371-e373.
- López Bravo A, Parra Soto C, Bellosta Diago E, Cecilio Irazola Á, Santos-Lasaosa S. (2019). Neurological manifestations of Behçet's disease: Case report and literature review. Reumatol Clin (Engl Ed). 15(5):e36-e38.
- el-Ramahi KM, al-Kawi MZ. (1991). Papilloedema in Behçet's disease: value of MRI in diagnosis of dural sinus thrombosis. J Neurol Neurosurg Psychiatry. 54(9):826-829.
- Wu Y, Yin W, Liu S, Wang S, Ding Y. (2023). Diagnosis and management of Neuro-Behçet disease with isolated intracranial hypertension: a case report and literature review. BMC Neurol. 23(1):335
- Lavalle S, Caruso S, Foti R, Gagliano C, Cocuzza S, La Via L, et al. (2024). Behçet's Disease, Pathogenesis, Clinical Features, and Treatment Approaches: A Comprehensive Review. Medicina (Kaunas). 60(4):562.
- Shokoohi S, Yaghoobi G. (2014). A rare case of Behçet's syndrome presenting with bilateral papillitis. Semin Ophthalmol. 29(2):77-79.
- Guney F, Bozkurt B, Paksoy Y. (2016). Intracranial Hypertension in Behcet Disease: A Case Report. J Clin Case Rep 6:748.
.png)