Previous Issues Volume 7, Issue 2 - 2024
Application of Prolotherapy for Pressure Injury
Kanav Gupta1, Ravi Kumar Chittoria2,*, Jacob Antony Chakiath3, Padmalakshmi Bharathi Mohan4
Senior Resident, Department of Plastic Surgery, JIPMER, Puducherry, India
Senior Professor and Associate Dean (Academic), Head of IT Wing and Telemedicine, Department of Plastic Surgery and Telemedicine, JIPMER, Puducherry, India
Senior Resident, Department of Plastic Surgery, JIPMER, Puducherry, India
Assistant Professor, Department of Plastic Surgery, JIPMER, Puducherry, India
*Corresponding Author: Ravi Kumar Chittoria, Senior Professor and Associate Dean (Academic), Head of IT Wing and Telemedicine, Department of Plastic Surgery and Telemedicine, JIPMER, Puducherry, India – 605006; Mobile: 9443133845; Email: [email protected]
Received Date: May 11, 2024
Publication Date: June 14, 2024
Citation: Gupta K, et al. (2024). Application of Prolotherapy for Pressure Injury. Mathews J Surgery. 7(2):33.
Copyright: Gupta K, et al. © (2024)
ABSTRACT
One of the complications seen in bedridden neurologically ill patients is pressure ulcers commonly known as pressure sores. Management of these ulcers is often challenging. But even after many wound therapies there is no well-established method that accelerates the wound healing rate. Prolotherapy entails injecting a local irritant into a wound with the purported aim of expediting healing. This article examines the significance of prolotherapy in preparing the wound bed for further skin cover procedures.
Keywords: Prolotherapy, Pressure ulcer, Management
INTRODUCTION
Pressure ulcers are frequently observed in critically ill patients, often necessitating grafts or other interventions for wound coverage. However, the preparation of the wound bed is crucial beforehand. Despite numerous therapies available for managing pressure ulcers, none have shown distinct advantages over others, making treatment challenging and time-consuming. Surgery might be necessary as a last resort to cover the raw area, but recurrence is common [1].
Moreover, reconstruction surgery may not be suitable for critically or chronically ill patients prone to pressure ulcers, hence conservative treatment is usually preferred.
Prolotherapy, among various local wound therapies, has been utilized for challenging wounds. It involves injecting or spraying an irritant into the wound to stimulate an inflammatory response believed to aid wound healing [2].
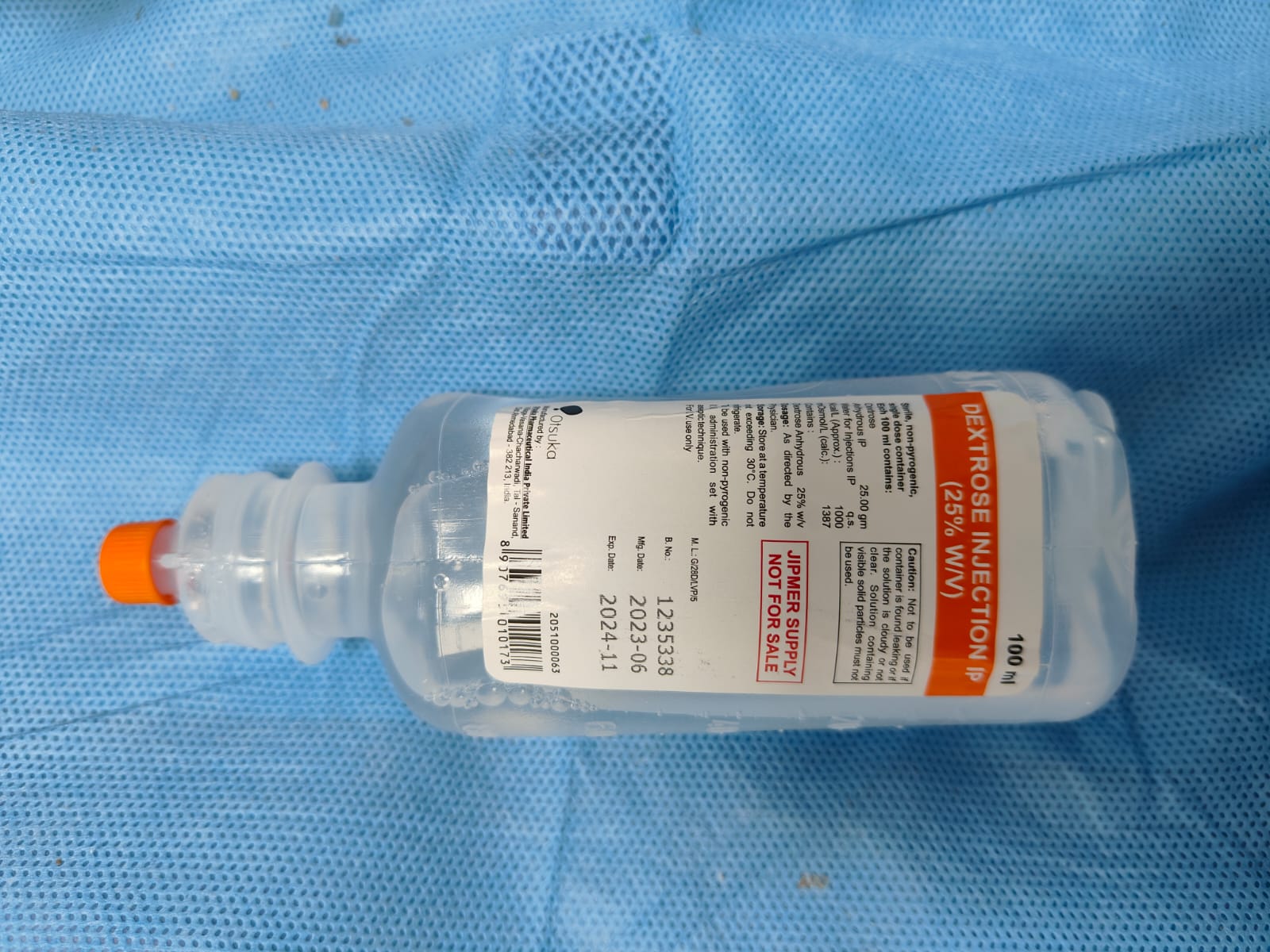
One of the commonly used agents in prolotherapy is dextrose, typically at concentrations between 12.5% to 25%. Dextrose is favored due to its water solubility, presence in blood chemistry, and safe injectability in large quantities.
Hypertonic dextrose solutions dehydrate cells at the injection site, causing local tissue trauma that attracts granulocytes and macrophages, promoting healing.
The most common prolotherapy agent used in clinical practice is dextrose, with concentrations ranging from 12.5% to 25%. Dextrose is considered to be an ideal proliferant because it is water soluble, a normal constituent of blood chemistry, and can be injected safely into multiple areas and in large quantity. In this article we share our experience of using prolotherapy in the pressure ulcer management.
METHODOLOGY
This is a case report of the use of prolotherapy in a case of non healing grade 4 pressure sores. This study was conducted in a tertiary care hospital in 2024.
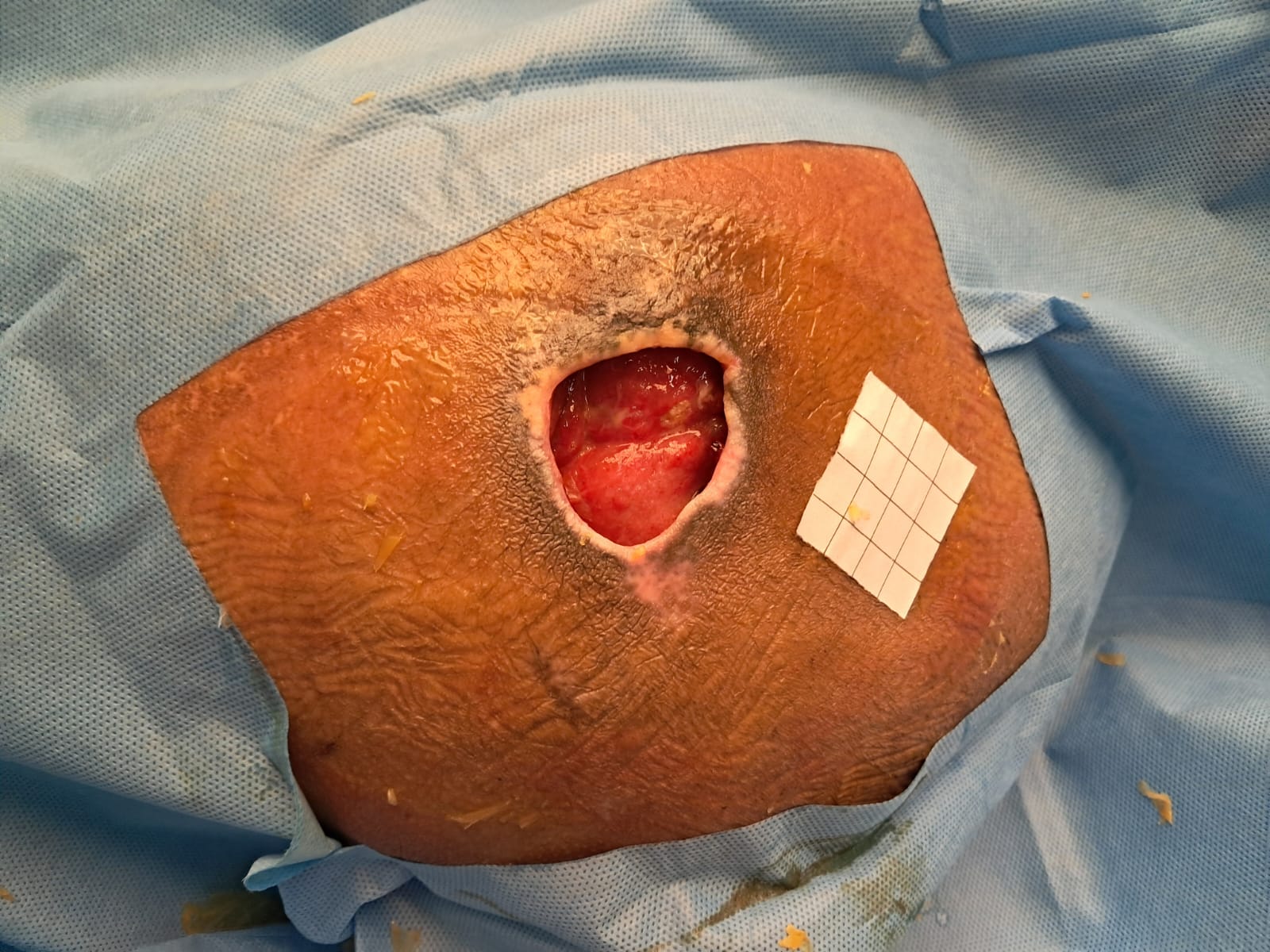
The patient was 66 year male with post-spinal cord injury with pressure ulcers on the right trochanteric region for 3 months (figure 1). The patient was thoroughly investigated both hematologically and radiologically. Wound tissue culture was sent and appropriate antibiotic therapy was given. Regular cleaning and dressing was done, but the wound was not showing any good sign of healing.
To hasten the wound bed preparation decision was made to give a trial of prolotherapy. In our case, we have used Dextrose 25% solution (figure 4) as an agent for prolotherapy (figure 2). It was spread evenly on to the wound followed by gauze dressing. A repeated session of prolotherapy was given every three days. After 3weeks of prolotherapy wound bed was prepared, wound was covered with granulation tissue, and size of the wound also decreased (figure 3).
RESULT
After six sessions of prolotherapy over three weeks period, the wound bed was prepared and reconstruction was planned (figure 1 and 3). No adverse local or systemic effect was noted with the use of prolotherapy. The Bates Jenson Wound Assessment Tool (BJWAT ) score decreased from 46 to 40, indicating improvement.
DISCUSSION
Pressure sore or ulcers occur at the area of prolonged contact with their site depending on position of the patient. The most common sites are-sacral region, heel, and occiput in the supine position, whereas the ischial region is the most common site in sitting position. Proper nursing care is required for its prevention. Once the pressure ulcer is developed, it is often hard to treat it. Often multi disciplinary team approach is required [1-3].
Various dressing methods have been advocated for pressure ulcer management, the prolotherapy is one such method. The term prolotherapy was coined by Dr. George Hackett in 1956. This word is derived from the Latin word proles meaning offspring or progeny and the English word- therapy. It involves injecting or applying an irritant substance (such as dextrose) to promote the growth of new tissue.
Multiple agents are used in prolotherapy, some classified as irritants (such as phenol), some as chemoattractants (commonly sodium morrhuate), and others as osmotic agents (commonly dextrose). Although the exact mechanism of prolotherapy is not clear, proponents of the technique believe that the injection of hypertonic dextrose causes cell dehydration and osmotic rupture at the injection site that leads to local tissue injury that subsequently induces granulocyte and macrophage migration to the site, with the release of the growth factors and collagen deposition.
In vitro studies have shown that even concentrations as low as 5% dextrose have resulted in the production of several growth factors critical for tissue repair. Some of these growth factors include PDGF, TGF-b, EGF, b-FGF, IGF-1, and CTGF 4. In Vitro studies have shown that the cultivation of cells in high glucose culture medium can increase PDGF expression. PDGF has multiple pro-reparative effects in skin wounds, including the promotion of angiogenesis, fibroblast proliferation, extracellular production. TGF-b expression is also upregulated by high glucose [5,6].
TGF-b is involved in all steps of wound healing including inflammation, angiogenesis, fibroblast proliferation, collagen synthesis, matrix deposition, and remodeling, and wound reepithelialisation. Other growth factors upregulated by high glucose include EGF, b-FGF, IGF, and CTGF, all having multiple preparative functions and improves healing in some animal Some studies on prolotherapy suggest that there are direct effects on collagen synthesis [7].
There is up-regulation of matrix in response to dextrose prolotherapy. Collagen expression is increased after exposure of patellar tendon fibroblasts to the prolotherapy agents dextrose and thus may contribute to tissue regeneration within a cutaneous wound. Collagen type-I synthesis is also increased in high-glucose cultivation of renal fibroblasts, in a TGF-b-mediated pathway. Changes in the cartilage matrix protein aggregation can is reported in chondrocytes cultured in high glucose, and in patients who have received intra-articular injections of 12.5% dextrose [4-8].
In our case we have used dextrose 25% as prolotherapy agent. We have used it as adjunct to other modalities. We have not noticed any adverse effect.
Figure 1: pre prolotherapy pressure sore on right trochanter ( BJWAT score 48).
Figure 2: while giving prolotherapy to pressure sore on right trochanter.
Figure 3: 3 weeks post prolotherapy to pressure sore on right trochanter ( BJWAT score 40).
Figure 4: 25% Dextrose used.
CONCLUSION
In this study, we found that prolotherapy has a role in the healing of the pressure ulcer and can be used as an adjuvant therapy for pressure ulcers. But since it is a single case study, a definite conclusion cannot be made. Large randomized control trials are required to confirm the efficacy of prolotherapy in pressure ulcer.
REFERENCES
- Mervis JS, Phillips TJ. (2019). Pressure ulcers: Pathophysiology, epidemiology, risk factors, and presentation. J Am Acad Dermatol. 81(4):881–890.
- Horn SD, Bender SA, Ferguson ML. (2004). The National Pressure Ulcer Long-term Care Study: pressure ulcer development in long-term care residents. J Am Geriatr Soc. 52:359–367.
- Mathus-Vliegen E. (2001). Nutritional status, nutrition and pressure ulcers. Nutr Clin Pract. 16:286–291.
- Oh JY, Choi GE, Lee HJ. (2018). High-glucose-induced reactive oxygen species stimulates human mesenchymal stem cell migration through snail and EZH2-dependent E-cadherin repression. Cell Physiol Biochem. 46:1749–1767.
- Penn JW, Grobbelaar AO, Rolfe KJ. (2012). The role of the TGF-β family in wound healing, burns and scarring: a review. Int J Burns Trauma. 2:18–28
- Freeman JW, Empson YM, Ekwueme EC, Paynter DM, Brolinson PG. (2011). Effect of prolotherapy on cellular proliferation and collagen deposition inMC3T3-E1 and patellar tendon f ibroblast populations. Transl Res. 158:132–139.
- Wu TJ, Fong YC, Lin CY, Huang YL, Tang CH. (2018). Glucose enhances aggre can expression in chondrocytes via the PK Calpha/p38-miR141–3p signalling pathway. J Cell Physiol. 233:6878–6887.
- Topol GA, Podesta LA, Reeves KD, Giraldo MM, Johnson LL, Grasso R, et al. (2016). Chondrogenic effect of intra-articular hypertonicdextrose (prolotherapy) in severe knee osteoarthritis. 8:1072–1082