Previous Issues Volume 1, Issue 2 - 2017
A Rare Case of a Small Bowel Obstruction Caused by a Ileal Neuroendocrine Tumor
Aleksandar R1 *, Vladimir R2 , Miroslav D1 , Arafeh M3 , Aleksandra Aleksic1 , Milan Gojgic1
1Clinical Hospital Center Bezanijska Kosa, Belgrade, Republic of Serbia.
2Emergency Center, Clinical Center of Serbia, Belgrade, Republic of Serbia.
3Cocoona Centre for Aesthetic Transformation, Dubai, UAE.
Corresponding Author: Aleksandar R, Hercegovacka 52b street, Belgrade 11080, Republic of Serbia, Tel: +381604646011; Email: [email protected]
Received Date: 08 Jun 2017
Accepted Date: 22 Jun 2017
Published Date: 26 Jun 2017
Copyright © 2017 Aleksandar R
Citation: Aleksandar R, Vladimir R, Miroslav D, Arafeh M, et al. (2017). A Rare Case OF a Small Bowel Obstruction Caused By a Ileal Neuroendocrine Tumor. Mathews J Surgery. 1(2): 008.
ABSTRACT
Small bowel Neuroendocrine tumors (SB-NET) are still a rare entity, even though their incidence is on a constant rise. Regardless of the fact that small bowel NET are more frequently being diagnosed on abdominal CT during medical check-ups, in high percentage of cases they are still being diagnosed during emergency surgery. We are presenting a case of an acute onset of small bowel obstruction generated from a Neuroendocrine tumor. The patient was admitted to the ICU, and after preoperative management, she was surgically treated for intestinal obstruction, with a small bowel resection, and a manual end-to-end anastomosis. The patient was released from hospital on the 13th postoperative day. Although major improvements have been made over the last years in the diagnosis and in the multimodal approach, and treatment of small bowel NETs, improving prognosis, the treatment of SB-NET still remains very challenging.
KEYWORDS
Neuroendocrine Tumor; Small Bowel Obstruction.
INTRODUCTION
Malignant tumors that are primarily located in small bowel are a very rare find. It is understood that their incidence is between 1% and 1.4% [1]. According to Yao et al. [2] there is a significant rise in the number of the newly diagnosed cases of Neuroendocrine tumors (NETs) of small bowel (SB-NET). An evaluation done by the Japanese pancreatic and gut NETs identified an increase in NETs by a factor of 1, 8 since 2005. Although there is an above mentioned significant rise in the number of newly established cases, since the symptoms and signs for small bowel-located primary malignant tumors are nonspecific, it is a very often occurrence that the diagnosis of SB-NET is established during emergency surgery for the acute onset of intestinal obstruction, perforation or, more seldomly, hemorrhage [3]. It is also important to point out that it is not rare that small bowel is secondarily involved by a tumor originating from adjacent organs or peritoneal carcinomatosis [4]. We are describing a case of a small bowel Neuroendocrine tumor with a clinical, and radiological findings of acute intestinal obstruction.
CASE REPORT
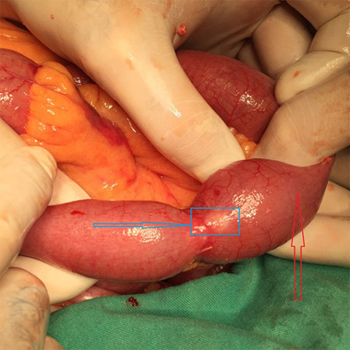
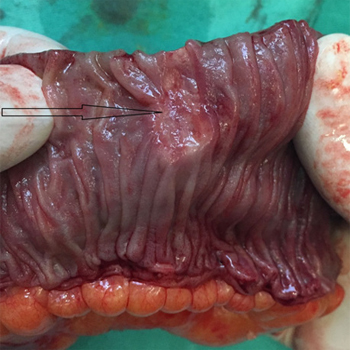
A 82-year old woman was admitted to our ER with a clinical, and radiological presence of an acute abdomen urgency. The patient presented with a history of 24h of vomiting, colicky like abdominal pain, abdominal distension, with no passage of flatus or stool for 48h. During her childhood, the patient was surgically treated for a case of acute appendicitis, while 15-years ago, she was submitted to open cholecystectomy and bile duct-radiographic exploration. Significant comorbidities were reported, firstly a long standing history of arterial hypertension, diabetes, as well as, Parkinson’s and Alzheimer’s disease. Upon physical examination diffuse abdominal pain, with guarding and rebound tenderness was found, along with abdominal distension, absence of bowel movement on auscultation, absence of flatus and stool, with significant nausea and vomiting. Blood tests revealed a normal WBC count, but with the elevation of CRP level (94, 2mg/l). The elevation of BUN (19, 3mmol/l), as well as creatinine (198umol/l), and potassium levels (6, 1 mmol/l) were also established. Abdominal X ray showed clear signs of bowel obstruction, while ultrasound described a substantial amount of free fluid in the abdominal cavity. Abdominal CT scan supported the findings of the above mentioned X-ray and ultrasound. No liver metastasis was established on the abdominal CT. After the preoperative treatment that included, NG tube placement, urine catheter insertion, two IV needles placement, rehidratation with crystalloid solutions, and administration of broad spectrum antibiotics, emergency surgery was performed. During the procedure a small bowel obstruction was diagnosed due to a Ileal stenosing mass. The patient was submitted to small bowel resection with the inclusion of the tumor mass, and a manual end-to-end anastomosis was performed. (Figure 1 and 2).
Figure 1: Intraoperative findings, with the blue arrow pointing out the small bowel-NET, with the red arrow pointing out dilated small bowel proximal to the location of NET.
Figure 2: Postoperative finding, after the performed small bowel resection, with the black arrow pointing out the NET.
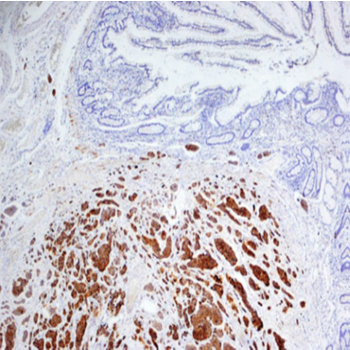
The histological report described a moderately-differentiated SB-NET which involved the mucosa, the sub mucosal level, and the retraction of the muscular layer. Immunohistochemistry (figure 3) revealed the following: The tumor cells showed a strong cytoplasmic immune reactivity to Chromogranin, Synaptophysin and CDX-2. The tumor cells did not reveal a positive reaction for CD 56, CK 7, CK 20 and CEA, while KI-67 was 10%.
Figure 3: Immunohistochemistry revealed the following: The tumor cells showed a strong cytoplasmic immune reactivity to Chromogranin, Synaptophysin and CDX-2. The tumor cells did not reveal a positive reaction for CD 56, CK 7, CK 20 and CEA, while KI-67 was 10%.
During the first five postoperative days, the patient was brad psychic and experienced tremor of the jaw and lips, as well as, tremor of both arms. All of which can be explained with the above mentioned history of Parkinson’s and Alzheimer’s disease. In alignment with the neurologist consultant, a slight modification of Madopar therapy was made. On the 6th postoperative day, the tremor was gone, while adequate bowel movement was established. The patient was released from hospital on the 13th postoperative day.
DISCUSSION
Neuroendocrine tumors are still a rare find, but one that it’s incidence is on a constant rise. It is widely considered that Neuroendocrine tumors are more common in female than in male patients. First description of a SB-NET was given by Oberndorfer and it dates back to 1907 [5]. The first thoughts on SB-NET were that they were lesions with malignant histological findings, but with no metastatic potential, which was overruled later on with Intraoperative and radiological findings. The induction in 1954 of 5-hydroxytryptamine aided in the diagnosis of NET [6]. Over the next couple of decades, the diagnosis of SB-NET constituted of clinical findings, serum and urinary markers, and radiology findings, predominantly with the induction of modern CT scanners. On CT SB-NET are usually described as hyper intense on the early arterial phase with a surrounding desmoplastic reaction, thought to occur because of the release of somatostatin [7].
A clear upgrade in the very diagnosis of SB-NET is the induction of pentetreotide single photon emission computed tomography (SPECT). The outlined advantage of this diagnostic procedure, is its ability of confirming that a lesion seen on CT is likely to, either be a NET or NET metastasis because of its uptake of pentetreotide and also to predict its potential response to peptide radio receptor therapy [8]. Although, the use of high-resolution imaging and endoscopy in clinical practice has resulted with the increase of early NET’s diagnosis, which favors good prognosis, a high percentage of SB-NET’s are still being diagnosed during emergency surgery for management of acute bowel obstruction, perforation and, more seldomly, hemorrhage. It is important to point out that around 6-30% of patients develop a clinical presentation which is typical for carcinoid syndrome, and it includes chronic diarrhea, flushing attacks, bronchial constriction to severe pulmonary spasm, carcinoid heart disease with arrhythmias, and hypo- or hypertension, and also abdominal pain/cramps. This syndrome is possible for serotonin, tachykinin and prostaglandin secreting NET’s, and when these products are not being activated by the liver. It is also considered that liver metastasis occurs in up to 90% of the cases [9]. The first line of management of SB-NET’s remains to be surgery. The surgical management is constituted of small bowel resection that involves the very tumor, and a end-to-end anastomosis of the bowel [10]. The metastatic potential of SB-NET is something that has been long evaluated in papers published in the past decades. Diffuse peritoneal or systemic spreading characterizes the palliative situation requiring surgery in a multimodal approach. A 5-year survival rate of 75% in patients treated multi modally for hepatic metastases from NETs in addition to a long-term octreotide-LAR therapy has been reported [11].
It is considered that a regional lymph node biopsy surrounding the origin of the superior mesenteric artery can be a significant parameter for the latter staging and therapy process. In conclusion, although major improvements have been made over the last years in the diagnosis and in the multimodal approach, and treatment of small bowel NETs, improving prognosis, the treatment of SB-NET still remains very challenging.
REFERENCES
- Hatzaras I, Palesty JA, Abir F, Sullivan P, et al. (2007). Small bowel tumors: epidemiologic and clinical characteristics of 1260 cases from the Connecticut tumor registry. Arch Surg. 142(3): 229-235.
- Yao JC, Hassan M and Phan A. (2008). One hundred years after ‘‘carcinoid’’: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 26: 3063-3072.
- Turan M, Karadayi K, Duman M, Ozer H, et al. (2010). Small bowel tumors in emergency surgery. Ulus Travma Acil Cerrahi Derg. 16(4): 327-333.
- Testini M, Trabucco S, Di Venere B and Piscitelli D. (2002). Ileal intussusception due to intestinal metastases from primary malignant melanoma of the lung. Am Surg. 68(4): 377- 379.
- Oberndorfer S. (1907). Carcinoid tumors of the duodenal arm. Frankf Z Pathol. 1: 426-432.
- Page IH. (1954). Serotonin (5-hydroxytryptamine). Physiol Rev. 34: 563-588.
- Boudreaux JP, Klimstra DS, Hassan MM, Woltering EA, et al. (2010). The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas. 39: 753-766.
- Kwekkeboom DJ, Kam BL, van Essen M, Teunissen JJ, et al. (2010). Somatostatin-receptor-based imaging and therapy of gastroenteropancreatic neuroendocrine tumors. Endoc Relat Cancer. 17: 53-73.
- Scherubl H, Faiss S and Zeitz M. (2003). Neuroendokrine gastrointestinal Tumore. Diagnostik und Therapie. Dtsch Med Wochenschr. 128: S81-S83.
- Scherubl H, Jensen RT, Cadiot G, Stolzel U, et al. (2010). Neuroendocrine tumors of the small bowels are on the rise: early aspects and management. World J Gastroenterol. 2(10): 325-334.
- Strosberg J, Gardner N and Kvols L. (2009). Survival and prognostic factor analysis of 146 metastaticneuroendocrine tumors of the mid-gut. Neuroendocrinology. 89: 471-476.