Previous Issues Volume 1, Issue 2 - 2017
Veno-Arterial Extracorporeal Membrane Oxygenation Using the Open Lung Approach for Ventilatory Support in a Case of Severe Acute Respiratory Distress Syndrome
Yoshitaka Hara1,Osamu Nishida1*,Hiroki Tsubouchi2,Tomoyuki Nakamura1,Naohide Kuriyama1,Daisuke Niimi3,Chizuru Yamashita1,Junpei Shibata1, Hidefumi Komura1
1Department of Anesthesiology and Critical Care Medicine, Fujita Health University School of Medicine, 1-98 Dengakugakubo, Kutsukake-Cho, Toyoake-city, Aichi, 470-1192, Japan.
2Department of Anesthesiology and Critical Care Medicine, Ichinomiyanishi Hospital, 1 Taira, Kaimei-Cho, Ichinomiya-City, Aichi 494-0001, Japan.
3Department of Anesthesiology and Critical Care Medicine, Nishichita General Hospital 3-1-1 Nakanoike, Tokai-city, Aichi 477-8522, Japan.
Corresponding Author: JOsamu Nishida, Department of Anesthesiology and Critical Care Medicine, Fujita Health University School of Medicine, 1-98 Dengakugakubo, Kutsukake-Cho, Toyoake-city, Aichi, 470-1192, Japan, Tel: +81-562-93-9008; E-Mail: [email protected]
Received Date: 07 Jul 2017 Accepted date: 17 Jul 2017 Published Date: 19 Jul 2017
Copyright © 2017 Osamu N
Citation: Osamu N, Hara Y, Tsubouchi H, Nakamura, et al. (2017). Veno-arterial Extracorporeal Membrane Oxygenation Using the Open Lung Approach for Ventilatory Support in a Case of Severe Acute Respiratory Distress Syndrome Mathews J Anesth. 1(2): 008.
ABSTRACT
Veno-venous (V-V) extracorporeal membrane oxygenation (ECMO) does not provide direct circulatory support, whereas veno-arterial (V-A) ECMO is reserved for severe circulatory failure. During ECMO, a mechanical ventilation setting with a strategy of lung rest is recommended, however, the specific setting is not clear. On the other hand, the beneficial effects of the open lung approach using a recruitment maneuver in patients with ARDS have been widely accepted and practiced as a lung-protective strategy. Here we report a case of ARDS associated with mild circulatory failure that was successfully treated by early veno-arterial (V-A) ECMO with high positive end-expiratory pressure (PEEP) as the open lung approach. This case indicates that this procedure may be effective for severe ARDS with preserved cardiac function.
KEYWORDS
Veno-Arterial Extracorporeal Membrane Oxygenation; Acute Respiratory Distress Syndrome; Open Lung Approach; Positive End-Expiratory Pressure; Recruitment Maneuver.
ABBREVIATIONS
V-V ECMO: Veno-venous extracorporeal membrane oxygenation, V-A: veno-arterial, ARDS: acute respiratory distress syndrome, CESAR: conventional ventilatory support versus ECMO for severe adult respiratory failure, PEEP: positive end-expiratory pressure
INTRODUCTION
Extracorporeal membrane oxygenation (ECMO) is considered effective for acute respiratory distress syndrome (ARDS) since the conventional ventilatory support versus ECMO for severe adult respiratory failure (CESAR) trial [1] and the H1N1 pandemic [2]. Generally, veno-venous (V-V) ECMO is the preferred mode for ARDS patients without circulatory failure. During ECMO, a mechanical ventilation setting with a strategy of lung rest is recommended, however, the specific setting is not clear. On the other hand, the beneficial effects of the open lung approach using a recruitment maneuver in patients with ARDS have been widely accepted and practiced as a lung-protective strategy. Here we report a case of ARDS associated with mild circulatory failure that was successfully treated by early veno-arterial (V-A) ECMO with high positive end-expiratory pressure (PEEP) as the open lung approach.
CASE PRESENTATION
A 51-year-old man with a history of depression, alcohol dependency and daily supplement use presented to our emergency department with general malaise after experiencing >20 vomiting episodes of black-brown food residue every 30-60 min. On arrival, he was in clinical shock, exhibiting paleness and cold sweats. His Glasgow Coma Scale score was 15, blood pressure 72/36 mmHg and heart rate 146 beats/min. A nasogastric tube was inserted, which drained copious black–brown fluid. Chest and abdominal X-ray and computed tomography findings were unremarkable. He was diagnosed with gastrointestinal bleeding, aspiration pneumonia, dehydration-induced hypovolemic shock and lactic acidosis (Table 1) and was transferred to the intensive care unit (ICU).
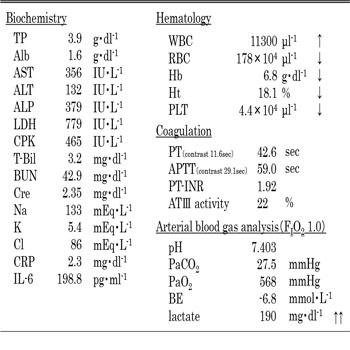
Table 1: Laboratory data on admission to ICU.
TP: total protein, Alb: albumin, ALP: alkaline phosphatase, T-Bil: total bilirubin, BUN: blood urea nitrogen, Cre: creatinine, IL: interleukin, PLT: platelet, PT: prothrombin time, APTT: activated partial thromboplastin time, AT-III: antithorombin III, INR: international normalized ratio
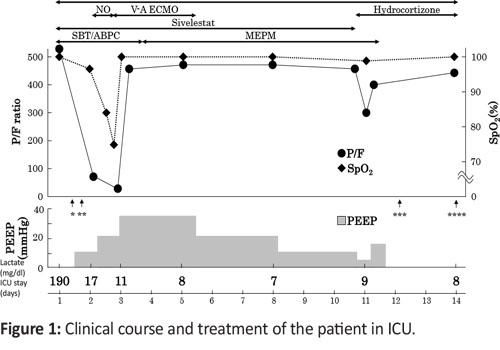
Emergent upper gastrointestinal endoscopy revealed only chronic gastritis, with no definitive bleeding source. Blood and fluid resuscitation and dopamine infusion at 2.5 μg/kg/min was initiated. His blood pressure and heart rate improved to 80/45 mmHg and 120 beats/min, respectively. Although the patient;'s P/F ratio was 568 on ICU admission, it deteriorated to 80.4 within 2 h, necessitating endotracheal intubation and mechanical ventilation. Sulbactam ampicillin was also commenced considering aspiration pneumonia and changed meropenem for intestinal bacterium including pseudomonas aeruginosa infection (Figure 1).
Figure 1: Clinical course and treatment of the patient in ICU.
PEEP: positive end-expiratory pressure, NO: nitric oxide, SBT/ABPC: sulbactam ampicillin, MEPM: meropenem, *: intubation, **: emergent gastrointenstinal fiberscope, ***: extubation, ****: ICU discharge.
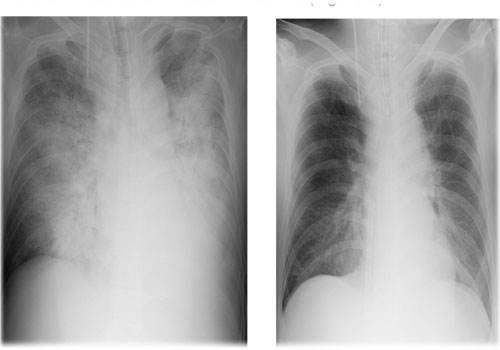
Subsequent echocardiography revealed good cardiac contractile force and almost no pericardial effusion. In the emergency department, chest X-rays revealed a cardiothoracic ratio (CTR) of 54.2%, similar to the 55.6% following loading infusion (Figure 2 (a). His central venous pressure was 11 mmHg under 10 cmH2 O PEEP, indicating noncardiogenic pulmonary edema. Severe ARDS was diagnosed according to the Berlin definition [3]. After 18 h in the ICU, his P/F ratio deteriorated to 64.3. PEEP was increased to 20 cmH2 O and nitrogen monoxide inhalation was added. However, his P/F ratio dropped to 50.9 after 24 h. We then decided to initiate V-A ECMO (Figure 2).
Figure 2: Chest radiograph
(a) Just before introduction to V-A ECMO, (b) After four days from the introduction of V-A ECMO.
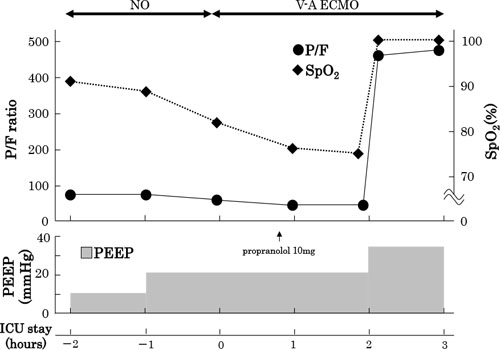
The ECMO circuit used was a CAPIOX® custom pack EBS SX type (TERUMO, Tokyo, Japan). A 16.5-French gauge (Fr) transdermal catheter was inserted into the left femoral artery for blood transmission, while a 21-Fr catheter was placed in the left femoral vein for blood drainage. Immediately after V-A ECMO initiation, the patient independently maintained cardiac output. His right-hand peripheral oxygen saturation (SpO2 ) and right radial artery P/F ratio were 74.4% and 42.2, respectively. Increasing PEEP (30-35 cmH2 O) as the open lung approach was implemented with concurrent low tidal volume management. Increasing PEEP reduced venous return and tended to decrease cardiac output. After that, his right-hand peripheral SpO2 and right radial artery P/F ratio improved to 100% and 408, respectively (Figure 3). This meant that V-A ECMO could supply sufficient oxygenated blood to his brain.
Figure 3: Clinical course, just before and after the introduction of V-A ECMO in ICU.
After the introduction of V-A ECMO, the SpO2 (right finger) did not increase because of high cardiac output. We intravenously infused propranolol 10 mg, however, the SpO2 did not improve. When the PEEP level increased up to 30 cm H2O as an open lung strategy, the SpO2 improved promptly. PEEP, positive end-expiratory pressure; NO, nitric oxide.
During V-A ECMO, his inspired oxygen fraction (FIO2) was 0.35, peak inspiratory pressure 35 cmH2O, PEEP 30 cmH2O (driving pressure 5 cmH2O), respiratory rate 3 breaths/min and inspiratory/expiratory ratio 1:2. V-A ECMO conditions were as follows: rotational speed, 2500 rotations/min; blood flow 3.6 L/min, CI 2.2 L/min/m2, ECMO O2 sweep gas 4.5 L/min and ECMO FIO2 1.0. On day 4 of V-A ECMO, blood flow decreased, his natural lung P/F ratio was 479, and chest X-ray improved (Figure 2 (b)), facilitating weaning from and stopping V-A ECMO. It was extubated on the 12th day. He was transferred to a regular ward on day 14 of admission and discharged without any morbidities in an ambulatory condition on day 17.
DISCUSSION
We reported the successful use of V-A ECMO using the open lung approach for severe ARDS with mild circulatory failure. V-V ECMO does not provide direct circulatory support, whereas V-A ECMO is reserved for severe circulatory failure. Furthermore, ventilator setting during V-V ECMO does not typically involve excessive recruitment maneuvers and high PEEP. In 2004, high PEEP was reportedly ineffective as part of the open lung approach for ARDS [4], this was contradicted by two subsequent studies [5, 6]. A meta-analysis about high PEEP revealed that ICU and hospital mortality rates were significantly decreased in patients with moderate ARDS (P/F < 200 mmHg) [7]. This suggests that the open lung approach is effective for severe ARDS requiring ECMO. The observation study was reported by Schmidt et al on the association between mechanical ventilation settings during ECMO and ICU mortality in three international (France and Australia) ECMO centers [8]. In multivariate analysis, higher PEEP levels during the first 3 days of ECMO support were associated with lower mortality (odds ratio, 0.75; 95% CI, 0.64–0.88; p = 0.0006). In contrast, Amato et al reported that among the various strategies for mechanical ventilation setting in ARDS, driving pressure, but not PEEP and tidal volume, was strongly associated with increased survival [9]. From these reports, high PEEP and low driving pressure on mechanical ventilation settings in ARDS suggest potential effectiveness. It is possible to perfuse blood with insufficient oxygen from the native heart to the brain, in case the respiratory function is very low and cardiac function is maintained like this patient. The reason is the confluence, where oxygenated blood through ECMO meets blood with low oxygen content from the heart, is more distal than the bifurcation area from arterial to brain tissue. V-V ECMO is recommended in such cases to avoid hypoxic encephalopathy. The possibility of hemodynamic collapse and barotrauma caused by high plateau pressure are pointed out as an adverse effect of high PEEP strategy. In this case, the patient received mechanical ventilation with high PEEP and low driving pressure without barotrauma and without concerns about circulatory collapse due to cardiac support by V-A ECMO. More specifically, high PEEP strategy as the open lung management for ARDS patients causes hemodynamic collapse. However, hemodynamic collapse during V-A ECMO for ARDS patients with relatively stable hemodynamic status may avoid hypoxic brain damage on account of sufficient oxygen delivery from ECMO (reduction of the relative cardiac output) to brain tissue in a retrograde fashion. Therefore, V-A ECMO with high PEEP during open lung ventilation may be useful for severe ARDS, although the optimal PEEP and plateau pressures remain open to discussion. Indeed, it remains unclear whether 30–35 cm H2O was adequate and whether the relatively short duration of high PEEP may have prevented barotrauma in the present case.
CONCLUSIONS
V-A ECMO using the open lung approach and high PEEP successfully controlled cardiac function in a case of severe ARDS without causing ventilator-associated lung injury, indicating that this procedure may be effective for severe ARDS with preserved cardiac function.
CONSENT
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
COMPETING INTERESTS
The authors report no conflicts of interest in this case report.
REFERENCES
- Peek GJ, Mugford M, Tiruvoipati R, Wilson A, et al. (2009). Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomized controlled trial. Lancet. 374(9698): 1351-1363.
- Davies A, Jones D, Bailey M, Beca J, et al. (2009). Extracorporeal Membrane Oxygenation for 2009 Influenza A (H1N1) Acute Respiratory Distress Syndrome. JAMA. 302(17): 1888-1895.
- Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, et al. (2012). Acute respiratory distress syndrome: the Berlin Definition. JAMA. 307(23): 2526-2533.
- Brower RG, Lanken PN, MacIntyre N, Matthay MA, et al. (2004). Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 351(4): 327-336.
- Meade MO, Cook DJ, Guyatt GH, Slutsky AS, et al. (2008). Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 299(6): 637-645.
- Mercat A, Richard JC, Vielle B, Jaber S, et al. (2008). Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 299(6): 646-655.
- Briel M, Meade M, Mercat A, Brower RG, et al. (2010). Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 303(9): 865-873.
- Schmidt M, Stewart C, Bailey M, Nieszkowska A, et al. (2015).Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome: a retrospective international multicenter study. Crit care med. 43(3): 654-664.
- Amato MB, Meade MO, Slutsky AS, Brochard L, et al. (2015). Driving pressure and survival in acute respiratory distress syndrome. N Engl J Med. 372(8): 747-755.