Previous Issues Volume 1, Issue 2 - 2017
Hemodynamic Response to Orotracheal Intubation: Bronchofibroscopy VS. Direct Laryngoscopy
Negrini D1*,Oliveira R2,Bethlem ED3
1Anesthesiology Service of the Gaffrée and Guinle University Hospital of the Federal University of the State of Rio de Janeiro (Universidade Federal do Estado de Rio de Janeiro).
2Discipline of Neuropsychiatry of the Federal University of the State of Rio de Janeiro.
3Cardiopulmonary Discipline of the Federal University of the State of Rio de Janeiro.
Corresponding Author: Negrini D, Anesthesiology Service of the Gaffrée and Guinle University Hospital of the Federal University of the State of Rio de Janeiro (Universidade Federal do Estado de Rio de Janeiro), Tel: +552123340639; E-Mail: [email protected]
Received Date: 28 Feb 2017 Accepted Date: 20 Apr 2017 Published Date: 21 Apr 2017
Copyright © 2016 Negrini D
Citation: Negrini D, Oliveira R and Bethlem ED. (2017). Hemodynamic Response to Orotracheal Intubation: Bronchofibroscopy VS. Direct Laryngoscopy. Mathews J Anesth. 1(2): 005.
ABSTRACT
Bronchofibroscopy is widely used in the context of orotracheal intubation in difficult airways. The cost of the equipment and the larger learning curve required compared to direct laryngoscopy increases its difficulty of use. Bronchofibroscopy may be less traumatic than direct laryngoscopy, triggering a lower hemodynamic response. Thus, we evaluated the behavior of heart rate and mean blood pressure in the process of orotracheal intubation by direct laryngoscopy and bronchofibroscopy in any airway scenario. Two groups of patients underwent orotracheal intubation by direct laryngoscopy (N = 32), group L, and bronchofibroscopy (N = 31), group B. These patients receiving elective surgeries at Gaffée and Guinle University Hospital (Hospital Universitário Gaffrée e Guinle – HUGG) were aged 18 years or older and did not have a full stomach. The predictors of difficult airways were evaluated during the pre-anesthetic evaluation, and the procedures were performed by the same anesthesiologist for both groups. All cases were performed under general anesthesia. Group L presented a rise in heart rate and mean blood pressure at the end of the procedure (p < 0.05), alterations not observed in group B. The duration of the procedure was higher in group B (p < 0.05). There was no intubation failure in any of the study patients. The absence of elevation in the parameters of heart rate and mean blood pressure in patients submitted to bronchofibroscopy orotracheal intubation compared to those intubated by direct laryngoscopy may be related to a lower nociceptive response and might lead to a broader indication of bronchofibroscopy in select clinical settings, regardless of the degree of airway difficulty.
INTRODUCTION
Although bronchofibroscopy is recognized as the gold standard for difficult airways [1-3], few studies have compared its efficacy and potential advantages over direct laryngoscopy in various scenarios of airway difficulty. In clinical practice, bronchofibroscopy is tacitly considered to be more efficient in cases of a difficult airway. However, it is questionable whether bronchoscopy is the most useful technique in cases of easy airway since most of the data on the subject is the result of guidelines, and the consensus of experts results from tradition rather than prospective, randomized and double-blind trials [4-6]. Hagberg and Artime refer to the bronchofibroscopy as the most widespread, versatile device since their development [7]. According to their research, bronchofibroscopy presents unique, superior characteristics to other devices, both in “awake” and anesthetized patients. There are also numerous clinical situations in which bronchofibroscopy is superior to other devices, including direct laryngoscopy. Bronchofibroscopy seems to have a lower hemodynamic repercussion and has the possibility of being performed at almost any position of the cervical spine [8]. This flexibility greatly facilitates intubation in patients who cannot have the cervical spine mobilized, and there are reports of bronchofibroscopy in the ventral decubitus [9]. However, the technique requires expertise and cannot be performed by all professionals, requiring a longer learning curve than direct laryngoscopy. In addition, bronchoscopy is not available in all hospitals. Rosenblatt et al. [10] argue that because of its higher cost and need for higher professional qualification, bronchofibroscopy should be reserved for predictably difficult airways. Revisions of algorithms from the American Society of Anesthesiology are in agreement. In support of this argument, Frova and Sorbello [11] did not demonstrate advantages of bronchofibroscopy over direct laryngoscopy in airway cases without predictors of difficulty. On the other hand the technique of direct laryngoscopy is the most used in clinical practice. Although it is not the most appropriate technique for predictably difficult airway and have potential to lead to elevation of heart rate and blood pressure, is the most widely used technique in the clinical practice. The reasons for this are the low learning curve, low cost and availability of equipment, short time for completing the procure and high success rate, which is explained in part by the low occurrence of difficult airways in the general population. Besides, it is considered that any elevation of heart rate and blood pressure parameters have no clinical significance in the vast majority of clinical scenarios. The hemodynamic variations resulting from orotracheal intubation correspond to the efferent arm of the vegetative reflex arc caused by the nociceptive stimulation inherent to the act of intubation. These variations occur in almost all patients submitted to direct laryngoscopy despite the use of drugs aimed at limiting it, such as opioids, local anesthetics and β-blockers. [12-14]. Although this hemodynamic response does not have major consequences for most patients, it may be deleterious in specific subgroups, such as, for example, in those with coronary disease. Variations of heart rate and blood pressure in response to nociceptive stimulation in the perioperative period are well known. Some authors suggest there are lower hemodynamic changes to orotracheal intubation when using a bronchofiberscope. [15] Confirmation of this fact could have an impact on the indication of the technique, at least in patients in whom such hemodynamic variations may be deleterious. [16] Heart rate and blood pressure variations are consistent, reliable autonomic markers of nociceptive activation. Elevated heart rate and increased blood pressure are strongly associated with the autonomic nervous system response to nociceptive stimuli. Another consideration concerns the technique of anesthesia usually used for orotracheal intubation by bronchofibroscopy. Most of the studies use the so-called “conscious sedation”, in which superficial sedation is performed so that the patient maintains the respiratory drive, airway protective capacity, and some capacity of interaction with the professional [17]. In addition to being more comfortable for the patient, performance of orotracheal intubation by bronchofibroscopy under general anesthesia reduces the hemodynamic response without hampering it, compared to intubation by an awake bronchofibroscope or by direct laryngoscopy. The loss of airway muscle tone resulting from general anesthesia requires special, generally simple maneuvers, such as anterior traction of the tongue with gauze [18] to allow visualization of the airway anatomy. Regarding the clinical evaluation of airway difficulty, there are two widely known usable criteria, one of which is clinically (Mallampati - table 1), and another assisted with laryngoscopy (Cormack-Lehane - table 2).
Table 1: Classification of Mallampati.
| Class I | Complete visibility of palatine tonsils, uvula and soft palate |
| Class II | Visibility of the soft palate, upper palatine tonsils and uvula |
| Class III | The hard and soft palate and the base of the uvula are visible |
| Class IV | Only the hard palate is visible |
Table 2: Classification of Cormack-Lahane.
| Grade 1 | Full view of the glottis |
| Grade 2 | Partial view of the glottis |
| Grade 3 | View of epiglottis only |
| Grade 4 | No visualization of glottis or epiglottis |
The advantages of bronchofibroscopy intubation in the difficult airways and the lower hemodynamic repercussion lead us to believe that this technique is more suitable for intubation, at least in certain subgroups of patients, regardless of the degree of difficulty of the airway and not only those classified as difficult. Therefore, the objective of this study was to compare the hemodynamic responses, measured through variations of heart rate and mean blood pressure, to orotracheal intubation by bronchofibroscopy and direct laryngoscopy under general anesthesia, regardless of the difficulty of intubation estimated by the classifications of Mallampati and Cormack and Lehane.
MATERIALS AND METHODS
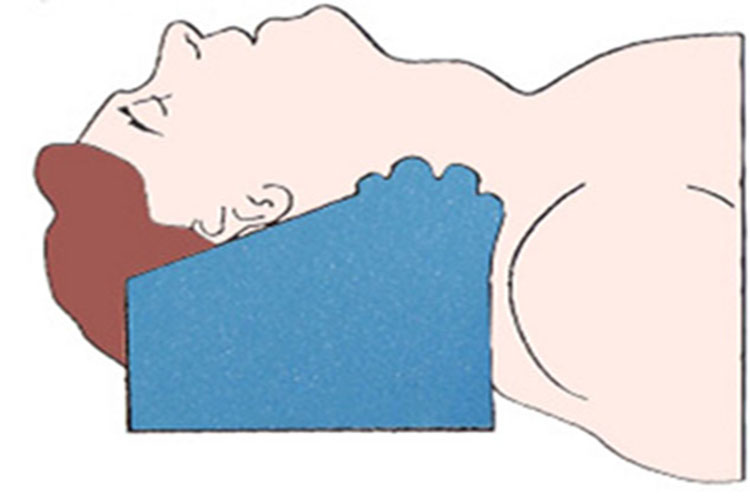
Adult patients who were 18 years old or older undergoing general anesthesia in elective surgery were included in this study. Exclusion criteria, in addition to those younger than 18 years, included patients with a “full stomach” (those in whom gastric emptying did not occur completely and there was a risk of regurgitation with the possibility of bronchoaspiration of gastric contents after anesthetic induction) and patients with contraindication of drugs chosen to induce general anesthesia. Patients or their legal guardians signed a written informed consent form prior to enrollment (Appendix A). The project was approved by the Ethics and Research Committee of the Gaffrée and Guinle University Hospital. All patients were initially assessed by using the Mallampati classification and submitted to the same standard head positioning (figure 1).
Followed by the following general anesthesia induction technique: 2 mg/kg propofol, 3 μg/kg fentanyl and 0.5 mg/kg atracurium, followed by ventilation with a facial mask and inhalation anesthesia with O2 and 2% sevoflurane for 5 minutes, a satisfactory time for all drugs to reach their peak serum concentration and action. Once the peak serum concentration of the anesthetic induction drugs was reached, we performed direct laryngoscopy in all patients, both in the direct laryngoscopy group (L group) and the bronchofibroscopy group (group B) to evaluate the Cormack-Lehane score, after which they were again ventilated under mask for another 2 minutes. At the end of this period, we performed orotracheal intubation by direct laryngoscopy or by bronchofibroscopy. To mark the time of the procedures, T1 was considered the beginning of the contact of the different devices with the oral cavity, and T2 was the exact moment that the capnography confirmed the correct positioning of the orotracheal tube in the airway. Statistical analysis of the results was performed by non-parametric methods given the non-Gaussian distribution of the variables of interest. The significance of the differences between the groups was estimated using the chi-squared test (X²) for categorical variables and the Mann-Whitney test (U) for dimensional variables. The strength of the correlations between dimensional variables was estimated by the Spearman correlation coefficient (rho). For all of the statistical tests, a significance level (a) of 0.05 was adopted.
RESULTS
A total of 63 patients were included, 32 in the L group (laryngoscopy) and 31 in the B group (bronchofibroscopy). The groups did not present significant differences regarding gender, age, color, weight or height (Table 3).
Table 2:Parameter comparisons within and between groups.
| Laryngoscopy | Bronchoscopy | Intergroup Comparisons | |
| N (W/M)a | 32 (18/14) | 31 (14/17) | X² = 0.77, p> 0.45 |
| Ageb | 49 ± 20 | 45 ± 17 | U = 434, p> 0.39 |
| Ethnicity(W/ NW)c | 18/14 | 14/17 | X² = 0.77, p> 0.45 |
| Weight (kg) | 72.7 ± 9.3 | 74.9 ± 11.7 | U = 450, p> 0.57 |
| Height (cm) | 168 ± 8 | 168 ± 7 | U = 443, p> 0.46 |
| T1-T2d | 26.4 ± 6.0 | 76.7 ± 16.3 | U = 0, p< 0.001 |
| HR T1e (bpm) | 72 ± 10 | 72 ± 12 | U = 492, p> 0.95 |
| FC T2f (bpm) | 82 ± 11* | 72 ± 9 | U = 277, p< 0.003 |
| MBP T1g (mmHg) | 75 ± 10 | 78 ±11 | U = 410, p> 0.23 |
| MBP T2h (mmHg) | 79 ± 11** | 77 ± 11*** | U = 437, p> 0.41 |
Aa Total number of participants (N): women (W) and men (M). b In full years. c Ethnicity: white (W) and non-white (NW). d T1-T2: Procedure execution time (in seconds). e HR T1: Heart rate immediately before the start of the procedure (T1). f HR T2: Heart rate immediately after the completion of the procedure (T2). g MBP T1: Mean blood pressure at T1. h MBP T2: Mean blood pressure at T2. Intra-group comparison ***Wilcoxon: Z = 4.35, p< 0.0001. ***Wilcoxon: Z = 3.66, p< 0.0001. ***Wilcoxon: Z = 2.13, p< 0.04.
Group B presented a longer procedure time than that of the L group (p < 0.001). The heart rate was higher in T2 in the L group compared to that in the B group (p < 0.003). Regarding the intra-group variations, the heart rate in the L group was higher in T2 (p < 0.0001). There was no difference in the heart rate in group B. The mean blood pressure (MBP) was higher in T2 in group L (p < 0.0001) and lower in T2 in group B (p < 0.04).
DISCUSSION
Bronchofibroscopy is recognized as more efficient and resolutive in scenarios where there are predictors of difficult airway, such as a high Mallampati classification (III or IV) [19,20,21]. However, this knowledge is essentially the result of the consensus of different societies and specialist expertise, rather than the result of studies designed to analyze the subject [22]. Bronchofibroscopy may be very useful even in the absence of predictors of difficult airway, that is, in the vast majority of patients undergoing general anesthesia with orotracheal intubation. Regarding this issue, it is usually assumed that bronchofibroscopy would require more time to be performed than direct laryngoscopy and would require greater expertise. Moreover, it would not be practicable by all anesthesiologists, and due to the high cost, the bronchofiberscope would not be available in all anesthesiology services. It is still assumed that both techniques would have equal success rates in the subgroup of patients without difficult airway predictors and that there would be no consequence of eventual elevation of heart rate and blood pressure when performing orotracheal intubation by direct laryngoscopy [23]. Considering this, we obtained two groups of patients, of whom 31 were submitted to orotracheal intubation by direct laryngoscopy and 32 by bronchofibroscopy. The groups were statistically identical in all of the anthropometric parameters studied (sex, age, color, weight and height) and incidence of difficult airway. They were also identical in their hemodynamic parameters (heart rate and MBP) at the beginning of the procedure. Finally, there were no intubation failures in any patient, that is, the success rate of the procedure was 100% in both groups. The time of orotracheal intubation was approximately three times longer in group B than that in group L. However, this time difference does not represent a significant risk in clinical practice because, although statistically significant, the increased time needed was short enough to not generate problems (1.3 minutes). The low occurrence of patients with difficult airway in both groups prevented statistical comparisons in this subgroup. In the L group, there was a significant increase in heart rate at T2 compared to that at T1, and there was no significant change in group B. Similarly, with regard to variations in MBP, the MBP was also higher at T2 in group L. These MBP observations were not noted in group B; curiously, the MBP was smaller at T2 than at T1, pointing to a lower hemodynamic stress and/or probable vagal response known to exist secondary to the bronchofibroscopic examination. There are few studies in the literature that address this issue in a similar way. Even with strong statistical significance, our observation is in disagreement with the study by Aghdaii N et al. [24], who did not demonstrate elevation of these two parameters in any of the two groups studied. In our opinion, this difference may have occurred because their study examined a specific population of patients undergoing myocardial revascularization surgery. As it is known, this group of patients makes continuous use of a series of medications, such as β blockers, among other drugs, capable of greatly attenuating elevations of the heart rate and blood pressure in response to any nociceptive stimulus. We believe that this limitation may have been an impediment to those researchers in observing differences between the two groups. In another study similar to ours, Barak M et al. [25] observed elevation in these two hemodynamic parameters in bronchofibroscopy and direct laryngoscopy groups. We believe that the reasons in this case are two-fold. First, the intubation procedures, including those of the bronchofibroscopy group, were performed by all anesthesiologists of the service, including those in training. For this reason, we believe that several of these patients were submitted to more traumatic procedures and with greater nociceptive activation than if all cases were performed by the same professional, in particular, a professional with more experience. In addition, there was no standardization in the choice of anesthetic induction drugs. Thus, some patients had more protective inductions of hemodynamic changes to the nociceptive stimulus of orotracheal intubation than others, making it difficult to compare the groups. Our experiment, on the other hand, corroborates the initial impression that orotracheal intubation by bronchofibroscopy does in fact yield lower hemodynamic repercussions in indicators such as heart rate, which could be explained by a lower response to the nociceptive stimulus of orotracheal intubation in group B. Similarly, with regard to variations in MBP, these observations are in line with the assumption that bronchofibroscopy is less traumatic and possibly generates less hemodynamic and nociceptive responses than laryngoscopy. It’s important to notice here that the eventually lower noceceptive response with brochofibroscopy is only a suggestion, based on the fact that there is a close and intimate correlation between hemodynamic changes, specifically in heart rate and mean arterial blood pressure and nociceptive response. More studies are needed to address this point in the future. All procedures in both groups were performed under general anesthesia because we considered it to be much more comfortable and less traumatic for the patients and professionals. The scientific community should consider the possibility of performing orotracheal intubation by bronchofibroscopy under general anesthesia and encourage the incorporation of this technique into the airway approach routine, as it is less traumatic. If intubation was performed in both groups with conscious sedation, the hemodynamic differences at T2 between the groups would be even greater since the hemodynamic response to direct laryngoscopy tends to be more pronounced under conscious sedation than under general anesthesia.
CONCLUSIONS
Orotracheal intubation by bronchofibroscopy tends to be less traumatic, with a lower hemodynamic response in heart rate and MBP than orotracheal intubation by direct laryngoscopy when performed under general anesthesia. This finding suggests that bronchofibroscopy is capable of inducing less nociceptive activation than direct laryngoscopy in orotracheal intubation.
Future Perspectives After confirmation of this fact with larger and better conducted studies, we envision expansion of the use of bronchofibroscopy beyond the context of the difficult airway. For example, this method could be part of the guidelines for anesthetic induction in elective surgeries in patients for whom these hemodynamic changes are considered undesirable and inappropriate, similar to the choice of drugs and other anesthetic techniques with that same objective in these specific subgroups of patients; namely, this recommendation may hold true regardless of the degree of airway difficulty predicted by the physical examination. We could predict a future in which we might consider to intubate a patient with brochofibroscopy based on the fact of his or her comorbidities, like coronary artery disease or any other condition in which changes in heart rate and mean arterial blood pressure may be undesirable, besides the degree of airway difficulty. Regarding this assumption, more studies are necessary in the future.
REFERENCES
- Hagberg CA, Artime CA and Daily WH. (2013). The difficult airway, a practical guideline. Flexible Fiberoptic Intubation. Chapter 9.
- Rodrigues AJ, Scordamaglio PR, Palomino AM, de Oliveira EQ, et al. (2013). Difficult airway intubation with flexible bronchoscope. Braz J Anesthesio. 63(4): 358-361.
- Levine AL and Leibowitz AB. (2013). Flexible bronchoscopy still the definitive standard for airway management. Anesthesiology. 118(2): 461.
- Artime CA, Hagberg CA and Daily WH. (2013). Flexible fiberoptic intubation. The Difficult Airway: A Practical Guide. Oxford: Oxford University Press. 97-108.
- Practice guidelines for management of the difficult airway: A report by the American Society of Anesthesiologists Task Force on management of the difficult airway. (1993)Anesthesiology. 78: 597-602.
- Avargués P, Cros AM and Daucourt V. (1999). Management of difficult intubation by French anaesthetists and impact of the French experts conference. Ann Fr Anesth Réanim. 18: 719-724.
- Hagberg CA and Artime CA. (2013). Airway Management in the Adult. Miller's Anesthesia. Chapter 55: 1647-1683.
- Cattano D and Cavallone L. (2011). Airway management and patient positioning: a clinical perspective. Anesthesiology News. 37: 17-23.
- Hung MH, Fan SZ, Lin CP, Hsu YC, et al. (2008). Emergency airway management with fiberoptic intubation in the prone position with a fixed flexed neck. Anesth Analg. 107(5): 1704-1706.
- Rosenblatt WH, Wagner PJ, Ovassapian A and Kain ZN. (1998). Practice patterns in managing the difficult airway by anesthesiologists in the United States. Anesth Analg. 87(1): 153-57.
- Frova G and Sorbello M. (2009). Algorithms for difficult airway management: A review. Minerva Anestesiol. 75(4): 201-209.
- Kord Valeshabad A, Nabavian O, Nourijelyani K, Kord H, et al. (2014). Attenuation of Hemodynamic Responses to Laryngoscopy and Tracheal Intubation: Propacetamol versus Lidocaine-A Randomized Clinical Trial. Anesthesiol Res Pract. 13: 1702-1747.
- Min JH, Chai HS, Kim YH, Chae YK, et al. (2010). Attenuation of hemodynamic responses to laryngoscopy and tracheal intubation during rapid sequence induction: remifentanil vs. lidocaine with esmolol. Minerva Anestesiol. 76(3): 188-192.
- Khan FA and Ullah H. (2013). Pharmacological agents for preventing morbidity associated with the haemodynamic response to tracheal intubation. Cochrane Database Syst Rev. 7(3): 1003-1007.
- Bruder N, Ortega D and Granthil C. (1992). Consequences and prevention methods of hemodynamic changes during laryngoscopy and intratracheal intubation. Ann Fr Anesth Reanim. 11(1): 57-71.
- Qi DY, Wang K, Zhang H, Du BX, et al. (2013). Efficacy of intravenous lidocaine versus placebo on attenuating cardiovascular response to laryngoscopy and tracheal intubation: a systematic review of randomized controlled trials. Minerva Anestesiol, 79(12): 1423-35.
- Kevin DJ and Mridula RR. (2013). Conscious sedation for awake fibreoptic intubation: a review of the literature. Can J Anesth, 60(6): 584-99.
- Kim SH, Woo SJ and Kim JH. (2010). Awake videolaryngoscopy-assisted tracheal intubation of the morbidly obese. Korean J Anesthesiol. 58(3): 249-55.
- Hagberg CA and Carin A. (2013). Benumof And Hagberg's Airway Management, Third edition.
- Stiles CM, Stiles QR and Denson JS. (1972). A flexible fiber optic laryngoscope. Jama. 221(11): 1246-1247.
- Kovacs G, Law AJ and Petrie D. (2007). Awake fiberoptic intubation using an optical stylet in an anticipated difficult airway. Ann Emerg Med. 49(1): 81-83.
- Koerner IP and Brambrink AM. (2005). Fiberoptic techniques. Best Pract Res Clin. Anaesthesiol. 19(4): 611-21.
- Ezri T, Szmuk P, Warters RD, Katz J, et al. (2003).Difficult airway management practice patterns among anesthesiologists practicing in the United States: have we made any progress? J Clin Anesth. 15(6): 418-22.
- Aghdaii N, Azarfarin R, Yazdanian F and Faritus SZ. (2010). Cardiovascular responses to orotracheal intubation in patients undergoing coronary artery bypass grafting surgery. Comparing fiberoptic bronchoscopy with direct laryngoscopy. Middle East J Anaesthesiol. 20(6): 833-38.
- Barak M, Ziser A, Greenberg A, Lischinsky S, et al. (2003). Hemodynamic and catecholamine response to tracheal intubation: direct laryngoscopy compared with fiberoptic intubation. J Clin Anesth. 15(2): 132-136.